Definition & Meaning
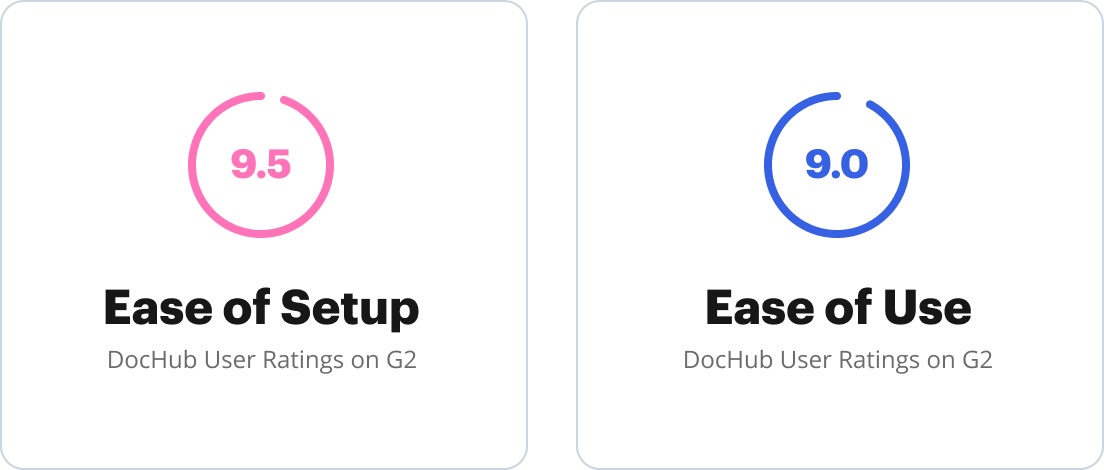
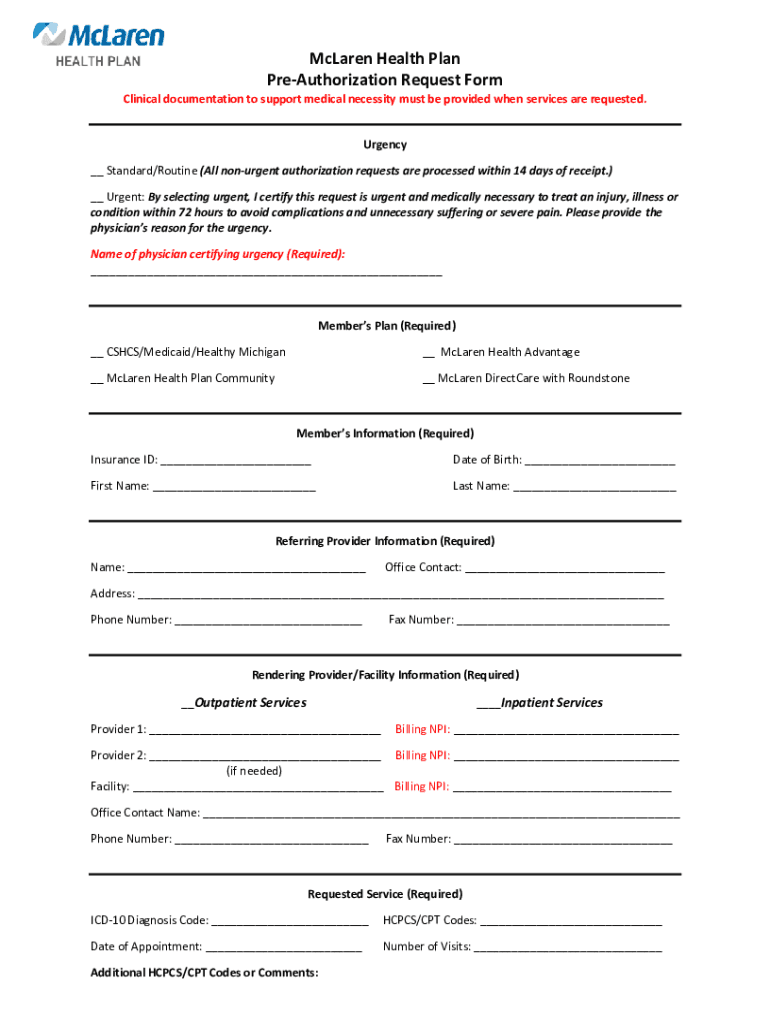
The McLaren authorization form is a document widely used within the healthcare community, specifically associated with the McLaren Health Plan. Its primary purpose is to gather important clinical documentation to substantiate the medical necessity of requested services. By using this form, healthcare providers can request approval for various medical procedures or treatments, ensuring they meet the insurance plan's criteria for coverage. The form includes essential details that range from patient information to specific diagnostic and procedure codes. It is crucial for the authorization of treatments that require prior approval from insurance payers to ensure they are covered under the patient's plan.
Key Elements of the McLaren Authorization Form
The McLaren authorization form consists of several critical sections that provide comprehensive information necessary for evaluating a authorization request:
-
Member and Provider Information:
- Includes the patient's personal details and their insurance identification number.
- Contains the provider's credentials, contact information, and the facility where services will be rendered.
-
Urgency Certification:
- A section dedicated to identifying whether the request is urgent or standard. Urgent requests often expedite the review process, allowing for quicker approvals.
-
Requested Services:
- Details specific services being requested, accompanied by ICD-10 diagnosis and CPT/HCPCS procedure codes. This information is essential for aligning the request with predefined medical criteria.
-
Confidentiality and Authorization Processes:
- Outlines the confidentiality terms concerning patient information.
- Describes the steps involved in obtaining authorization, ensuring all parties understand the process and legal requirements.
How to Obtain the McLaren Authorization Form
Obtaining the McLaren authorization form involves several straightforward methods that enhance accessibility for healthcare providers and patients:
-
Online Access:
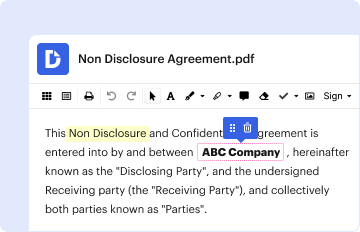
- The form is typically available on the McLaren Health Plan's official website. This option allows users to download a digital version, which can be filled out electronically.
-
Through Providers:
- Healthcare providers affiliated with McLaren can provide the form directly to patients in need of pre-authorization for services.
-
Customer Support Assistance:
- McLaren Health Plan's customer service department can be contacted to request a physical or digital copy of the form, delivering it via mail or email as per user preference.
Steps to Complete the McLaren Authorization Form
The process of completing the McLaren authorization form is meticulous, ensuring all details are accurately filled out to facilitate a seamless review:
-
Enter Member and Provider Information:
- Input all necessary details for both the patient and the healthcare provider. Ensure accuracy, as discrepancies can lead to delays in the authorization process.
-
Specify the Requesting Services:
- Clearly state the medical services or procedures needing authorization, including specificity in diagnosis and procedure codes.
-
Certify Urgency Level:
- Determine and certify whether the request is urgent. Use this designation carefully, as it impacts resource allocation and speed of response.
-
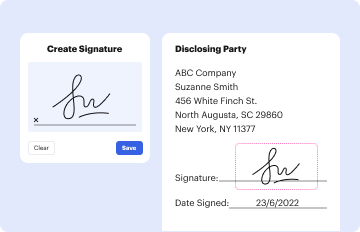
Review and Sign:
- Carefully review the entire form for completeness and accuracy. Once confident, sign the form. Both the provider and patient may need to provide signatures to validate the request.
Important Terms Related to the McLaren Authorization Form
Understanding industry-specific terminology is vital when dealing with McLaren authorization forms:
- Medical Necessity: A healthcare service or product that is reasonable and necessary for the diagnosis or treatment of illness or injury.
- ICD-10 Codes: The International Classification of Diseases, Tenth Revision, used to classify and code all diagnoses, symptoms, and procedures.
- CPT/HCPCS Codes: Current Procedural Terminology (CPT) and Healthcare Common Procedure Coding System (HCPCS) codes used to describe medical, surgical, and diagnostic procedures and services.
- Primary Payer: The health insurance plan responsible for processing claims first, before other plans become liable.
Legal Use of the McLaren Authorization Form
The McLaren authorization form is legally significant in the healthcare field, directly impacting how services are preapproved and paid for by insurance:
- Compliance with Insurance Policies:
- Ensures services are in line with specific health plan terms before services are rendered.
- Regulatory Approval:
- Compliance with industry regulations and healthcare laws when using this form is crucial for maintaining legal integrity in the authorization process.
Providers and patients must accurately complete and submit the form to avoid breaches in contract and coverage denials.
Form Submission Methods
Submitting the McLaren authorization form can be done through various methods, each offering different conveniences:
-
Electronic Submission:
- Forms completed digitally can be emailed or uploaded through McLaren's online portal for faster processing.
-
Mail Submission:
- Physical forms can be mailed directly to McLaren Health Plan, though this method may take longer than electronic submissions.
-
In-Person Submission:
- Some providers may allow patients to submit the form in person, enabling immediate review and feedback.
Choosing the appropriate submission method is critical for timely processing and receiving the necessary pre-approval for medical services.
Who Typically Uses the McLaren Authorization Form
The McLaren authorization form is primarily used by individuals and entities within the healthcare and insurance sectors:
-
Healthcare Providers:
- Doctors, specialists, and medical facilities utilize the form to secure approval for procedures and treatments that require pre-authorization.
-
Patients:
- Individuals requiring medical services that necessitate prior insurance consent will interact with the form to ensure coverage.
-
Insurance Professionals:
- These professionals assist in evaluating the authorization forms to determine the medical necessity and align them with available health plan benefits.
These key user groups ensure that medical services comply with insurance requirements and maintain eligibility for coverage.