Definition and Overview of Discharge Summary OT
The discharge summary for occupational therapy (OT) is a formal document that encapsulates a patient's therapeutic journey and progress throughout their treatment period. It serves critical functions in conveying the essential details surrounding a patient's care, including their admission status, the long-term goals (LTGs) established, and the outcomes achieved upon discharge. This document is essential for healthcare providers, patients, and any future caregivers, ensuring continuity of care and adequate follow-up.
The discharge summary typically specifies whether each targeted goal was met and provides rationales for discharge decisions—such as achieving individual goals or reaching the maximum potential for improvement through the intervention. Additionally, this document often contains recommendations for post-discharge care, including home exercise programs, medical follow-ups, and necessary referrals to other healthcare professionals. The therapist's contact information is also included for any future inquiries or clarification.
Key Elements Included in the Discharge Summary OT
An effective discharge summary OT includes several key components, ensuring comprehensive coverage of the patient's condition and treatment:
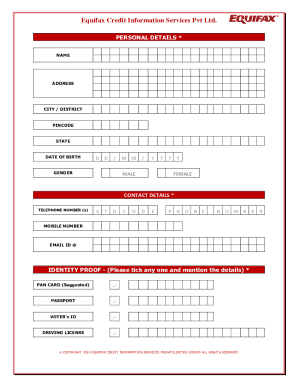
- Patient Information: Name, demographics, and relevant medical history.
- Dates of Service: Admission and discharge dates to document the timeline of therapy.
- Therapy Goals: Enumeration of the long-term goals set at the beginning of therapy and the status of each goal upon discharge.
- Goals may include improving mobility, enhancing daily living activities, or increasing strength and flexibility.
- Summary of Progress: A detailed narrative outlining the patient's progress throughout therapy sessions, including the types of interventions utilized.
- Reasons for Discharge: Justifications for concluding therapy, which may include goal achievement or specific clinical criteria being met.
- Recommendations: Suggestions for ongoing care or follow-up appointments, ensuring the patient continues to receive support as needed.
Including thorough details in these categories helps create a robust record that can be referenced by various stakeholders in the patient's healthcare journey.
Steps to Complete the Discharge Summary OT
Completing a discharge summary OT involves systematic steps to ensure accuracy and completeness:
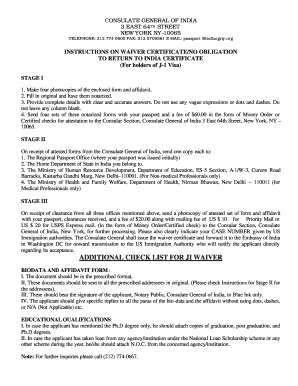
- Gather Patient Information: Collect the patient's full name, date of birth, and any pertinent medical history.
- Review Therapy Goals: Assess the established long-term goals and document the final status of each, noting if they were met, along with supporting details.
- Document Sessions: Summarize the therapy sessions, describing techniques employed and patient engagement levels to provide context for the patient's progress.
- Provide Reason for Discharge: Clearly articulate the rationale behind the decision to discharge the patient from therapy. Emphasize achievements and readiness for discharge.
- Include Recommendations: Specify any additional resources, activities, or follow-up appointments that may benefit the patient after discharge.
- Finalize the Summary: Ensure all sections are complete and accurate, and sign the document to validate the information provided.
By following these steps, clinicians can create a clear, informative record that enhances continuity of care.
Legal Considerations and Compliance for Discharge Summary OT
The discharge summary OT must comply with various legal and regulatory standards to ensure it is recognized as a valid document in healthcare settings:
- Patient Privacy: Compliance with HIPAA regulations is critical. The summary should only share information pertinent to the patient's therapy and care, safeguarding privacy.
- Legal Binding: This document may serve as legal evidence of the treatment provided and the rationale for discharge. Therefore, it must be accurate and reflect the care delivered.
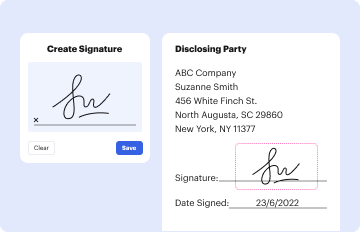
- Signature and Date: The summary should include the therapist's signature and the date of completion to validate its authenticity.
Understanding these legal aspects is fundamental for practitioners to protect both themselves and their patients.
Practical Examples of Discharge Summary OT Usage
Discharge summaries for occupational therapy can vary significantly based on the patient population and treatment focus. Notable examples include:
- Post-Stroke Rehabilitation: A discharge summary may document mobility goals achieved, indicating the patient can perform specific activities of daily living independently, which is crucial for their return home.
- Pediatric OT Cases: For children with developmental delays, the summary might detail improvements in fine motor skills and social interactions, along with recommendations for home-based support activities.
- Geriatric Patients: In elderly patients recovering from surgeries, the summary can highlight progress in balance and coordination, detailing recommended fall-prevention strategies for independent living.
These practical applications illustrate how discharge summaries can be tailored to reflect diverse patient needs and therapy goals effectively.
Importance of Recommendations in the Discharge Summary OT
Providing clear recommendations in the discharge summary OT is essential for maintaining patient care post-discharge. These recommendations should be:
- Specific: Outline precise home programs or strategies to build on the gains made during therapy.
- Feasible: Ensure that the recommendations are actionable and align with the patient’s capabilities and environment.
- Measurable: Include criteria that help assess the patient’s progress in follow-up appointments, such as frequency and types of exercises to perform.
Including well-thought-out recommendations helps empower patients in their recovery process and optimizes the effectiveness of occupational therapy beyond discharge.