Gain access to ready-made customizable Anthem new provider Application Forms forms. Create and organize your templates on the go with DocHub flexible online tools.


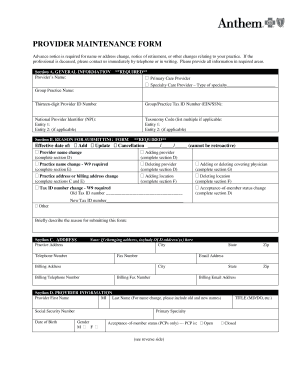

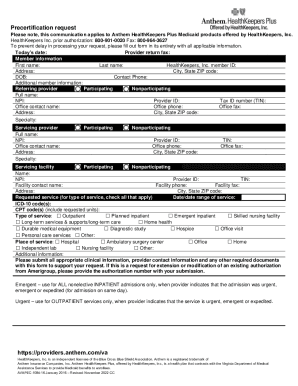

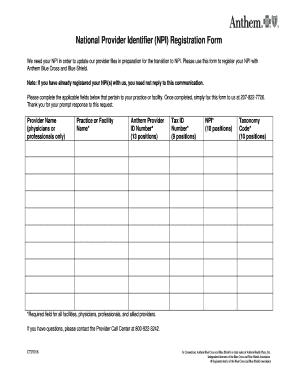
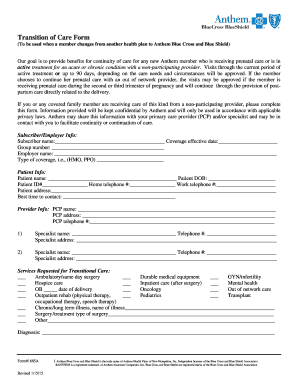



Document management can overpower you when you can’t locate all the forms you need. Luckily, with DocHub's extensive form library, you can find everything you need and promptly take care of it without changing between applications. Get our Anthem new provider Application Forms and begin working with them.
How to use our Anthem new provider Application Forms using these easy steps:
Try out DocHub and browse our Anthem new provider Application Forms category without trouble. Get a free profile today!