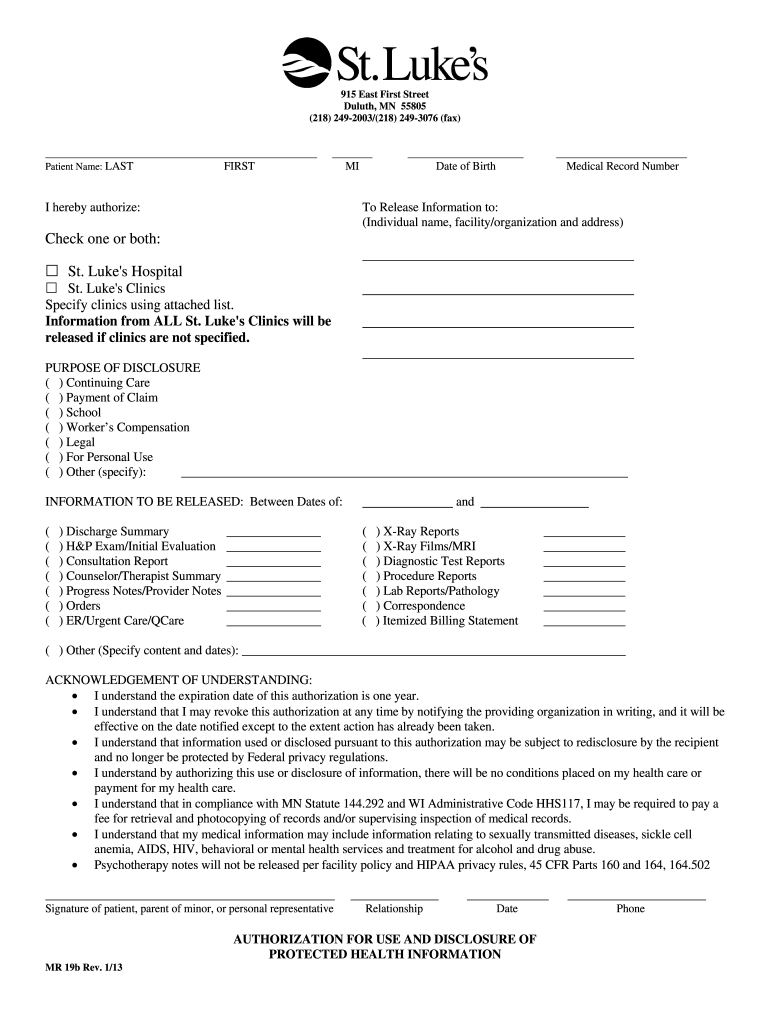
Definition and Meaning of Hospital Discharge Papers
Hospital discharge papers are critical documents provided to patients upon their release from a hospital. They serve as a formal record of a patient's hospital stay, including details about the diagnosis, treatments received, and instructions for post-hospital care. These papers may include information that is vital for follow-up appointments, physical therapy, medication management, and understanding the ongoing care required after discharge.
Discharge papers are also known as discharge summaries or discharge instructions. They typically outline the specific reasons for hospitalization, the procedures or interventions performed, and the patient's current condition. The overall goal of these documents is to ensure that patients have a clear understanding of their health status and the steps they need to take moving forward.
Key Components of Hospital Discharge Papers
- Patient Information: Name, date of birth, and hospital identification number.
- Admission and Discharge Dates: The duration of the hospital stay.
- Diagnosis: The medical conditions being treated.
- Treatments Provided: Procedures and medications administered during the hospital stay.
- Instructions for Home Care: Recommendations for medications, physical activity, and dietary modifications.
The clarity and comprehensiveness of hospital discharge papers are essential in promoting patient safety and ensuring effective transitions of care.
How to Obtain Hospital Discharge Papers
Patients can obtain their hospital discharge papers either during their discharge process or afterward. Here’s a step-by-step guide on how to secure these documents:
-
During Discharge:
- Patients should request their discharge summary from the healthcare team before leaving the hospital.
- Most hospitals have a standardized process where the nursing staff or discharge planner will review the documents with the patient and family.
-
Contacting the Hospital:
- If the papers are not obtained at discharge, patients can contact the hospital's medical records department.
- It's important to provide identifying information, such as the patient's full name, date of birth, and date of hospital stay.
-
Using Patient Portals:
- Many hospitals offer electronic health record (EHR) systems that allow patients to access their discharge papers online.
- Patients should log in to their healthcare provider's patient portal, navigate to their visit history, and download the discharge summary.
-
Requesting via Mail or Fax:
- For security and privacy reasons, some patients may need to submit a formal request in writing to receive a copy of hospital discharge papers by mail or fax.
Steps to Complete Hospital Discharge Papers
Completing hospital discharge papers requires careful attention to detail to ensure all relevant information is accurately recorded. Here are the general steps involved:
-
Gather Necessary Information:
- Collect all patient data, including personal identification and health history.
- Review the hospital stay, including diagnoses and treatments.
-
Fill in Patient Details:
- Accurately input the patient's name, contact information, and hospital identification number.
- Document the admission and discharge dates.
-
Detail Medical History:
- Summarize the patient’s medical history leading to hospitalization and any pre-existing conditions.
-
Outline Treatments and Medications:
- List all medications administered during the hospital stay, including dosages and administration schedules.
- Include significant procedures and interventions performed during the hospital stay.
-
Provide Post-Discharge Instructions:
- Clearly outline any recommendations for medication, follow-up appointments, and lifestyle modifications.
- Address any signs or symptoms requiring immediate attention after discharge.
-
Review and Validate Data:
- Confirm that all information is complete and accurate.
- Obtain necessary signatures from relevant healthcare providers to validate the document.
Legal Use of Hospital Discharge Papers
Hospital discharge papers serve a legal purpose in the healthcare system, ensuring adequate documentation of a patient's medical history and treatment. Their legal significance includes the following:
- Continuity of Care: They serve as a legal record that supports continuity of care between healthcare providers.
- Liability Protection: Ensures hospitals and healthcare providers are protected from potential legal liability through thorough documentation of care provided.
- Insurance Claims: Essential for verifying treatments and facilitating insurance claims processing.
- Patient Rights: Discharge papers empower patients by outlining their rights, responsibilities, and the information needed for ongoing care.
Understanding the legal implications of these documents is crucial for both health professionals and patients, ensuring compliance and protection in healthcare practices.
Examples of Hospital Discharge Papers
To understand hospital discharge papers better, here are examples of what these documents might include:
-
Sample Discharge Summary: A document detailing the patient's hospitalization, stating the diagnosis (e.g., pneumonia) and treatments (e.g., antibiotics, respiratory therapy), followed by instructions for home care.
-
Discharge Instructions Example: A separate document outlining the medications prescribed at discharge, such as dosages and frequency, along with guidance on when to seek medical attention and recommendations for follow-up appointments.
-
Case Studies: Real-world scenarios illustrating how clear discharge documents aided recovery, including patient feedback on the usefulness of the information provided.
The illustrative examples aid both patients and healthcare providers in ensuring all necessary components are included in hospital discharge papers, fostering improved patient outcomes.
Important Terms Related to Hospital Discharge Papers
Familiarity with terminology related to hospital discharge papers is essential for proper understanding and communication regarding post-discharge care. Key terms include:
- Discharge Plan: A strategic outline created by healthcare providers that details how a patient will transition from hospital to home.
- Follow-Up Care: Medical care provided after the discharge, which may involve visits to primary care physicians or specialists.
- Aftercare: Ongoing care that a patient must follow, often specified in discharge instructions, including medication adherence, physical therapy, and lifestyle changes.
- Patient Education: Information provided by healthcare providers to help patients understand their diagnosis and treatments, included in discharge paperwork to enhance compliance.
Defining these terms promotes clarity in discussions and documentation, ensuring that patients and care providers have a mutual understanding of responsibilities and expectations after discharge.