Definition & Purpose of Iowa Medicaid Enterprise
The Iowa Medicaid Enterprise (IME) operates within the Iowa Department of Human Services and is responsible for administering the Medicaid program in Iowa. This program is crucial for providing healthcare coverage to low-income individuals and families, as well as elderly and disabled persons who meet specific eligibility criteria. IME aims to ensure comprehensive healthcare coverage, improve health outcomes, and manage healthcare costs effectively. By understanding the purpose and scope of IME, stakeholders can optimize the use of healthcare resources and navigate the Medicaid landscape efficiently.
How to Use the Iowa Medicaid Enterprise - Iowa Department of Human Services
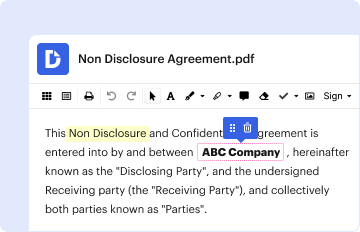
Using the services provided by IME involves several steps, which are crucial for accessing Medicaid benefits in Iowa. Initially, individuals should assess their eligibility through the Department of Human Services (DHS) guidelines. Once eligibility is confirmed, potential beneficiaries can apply for Medicaid through the DHS website or by visiting local offices for assistance. After enrollment, users can select their healthcare providers and manage their benefits through the IAM system, which provides a centralized platform for Medicaid-related information and resources.
Steps to Complete the Iowa Medicaid Enterprise Application
Completing the IME application involves a systematic process. First, gather all required documents, including proof of income, residency, and identity. Next, visit the DHS website or local office to complete the application form. Make sure to fill out all sections accurately to avoid delays. After submission, a DHS representative reviews the application and may request additional information. Finally, once approved, beneficiaries receive a Medicaid card and instructions on accessing services.
Eligibility Criteria for Iowa Medicaid
Eligibility for Medicaid under the IME depends on several factors, including income level, family size, age, disability status, and specific health needs. For instance, children, pregnant women, low-income adults, and those with disabilities are primary candidates. Income thresholds vary based on federal poverty guidelines, making it important for applicants to review current criteria. Additionally, some programs require participants to provide proof of medical necessity to receive certain benefits.

Important Terms Related to Iowa Medicaid
Understanding key terms related to IME is essential for effective participation in the program. Terms like "Managed Care Organization" (MCO), "Fee-for-Service," and "Notice of Action" are frequently encountered. MCOs refer to the groups that manage Medicaid services, offering networks of healthcare providers. Fee-for-Service is a payment model where services are billed separately, while Notice of Action is an official communication about changes to benefits or services. Familiarity with these terms helps in navigating the Medicaid system competently.
Legal Use of the Iowa Medicaid Enterprise Services
Navigating legal aspects is crucial when utilizing IME services. Beneficiaries must use Medicaid funds solely for approved healthcare services and adhere to program rules. Fraud or misuse, such as providing false information or sharing Medicaid cards, is subject to penalties. Furthermore, appealing decisions about coverage or services follows a formal process, safeguarding beneficiaries' rights to dispute changes or denials.
Key Elements of the Iowa Medicaid Enterprise - Department of Human Services Program
IME incorporates several core elements to provide comprehensive healthcare services. These include the implementation of MCOs to streamline service delivery, the integration of health data systems for efficient management, and the collaboration with healthcare providers to ensure service accessibility. Furthermore, IME emphasizes preventive care and chronic disease management, supporting a holistic approach to health that reduces overall costs while improving quality of life for Medicaid recipients.
Software Compatibility and Integration with Iowa Medicaid Enterprise
IME services integrate seamlessly with various software tools to enhance user experience and operational efficiency. Health apps and digital platforms can synchronize with Medicaid systems, allowing users to access benefits, schedule appointments, and manage care plans online. Compatibility with systems like TurboTax or QuickBooks is possible for financial reporting and compliance, although specifics depend on the software's flexibility and the user's needs. Employing compatible software solutions facilitates efficient management of healthcare and financial responsibilities related to Medicaid services.