Definition and Purpose of the BCBS Reconsideration Form in Florida
The BCBS reconsideration form in Florida, often referred to as the Florida Blue reconsideration form, serves as a crucial tool for healthcare providers to challenge post-service claim processing decisions made by Florida Blue, part of the Blue Cross Blue Shield (BCBS) network. This form allows providers to request a review or reconsideration of a claim that has already been processed and denied, ensuring that they have an opportunity to present further information or clarify issues that may have led to the denial.
Key Functions of the BCBS Reconsideration Form
- Appeal of Denial: The primary function is to formally appeal a claim denial, offering a structured way to present additional information or corrections.
- Documentation Submission: Providers can attach supporting documents that substantiate the claim being reconsidered.
- Deadline Compliance: The form must be submitted within a specific time frame, typically within one year from the date of the remittance advice, ensuring that appeals are processed promptly.
How to Obtain the BCBS Reconsideration Form in Florida
To effectively engage in the reconsideration process, obtaining the required form is essential. Healthcare providers can access the BCBS reconsideration form through several channels.
Methods to Access the Form
- Florida Blue Website: Providers can download the form directly from the official Florida Blue website. Look for the resources section dedicated to providers.
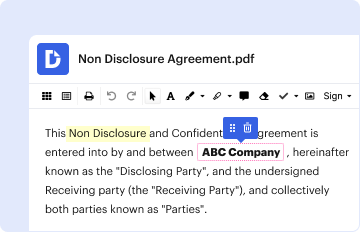
- Provider Portals: Many providers manage their claims through an online portal provided by Florida Blue, which often includes access to necessary forms.
- Contacting Florida Blue: Providers can also request the form by contacting Florida Blue customer service directly, ensuring they receive the most current version.
Steps to Complete the BCBS Reconsideration Form in Florida
Completing the BCBS reconsideration form accurately is vital for a successful appeal. Below are detailed steps to guide providers through the process.
Instructions for Form Completion
-
Personal Information:
- Fill in the provider's name, NPI number, and contact information accurately at the top of the form.
-
Claim Information:
- Clearly indicate the claim number being appealed and the date of service. This ensures that the proper records are identified.
-
Reason for Reconsideration:
- Provide a detailed explanation of the reasons for the appeal. Include any relevant facts or circumstances—this section is crucial as it forms the basis of the reconsideration request.
-
Supporting Documentation:
- Attach all necessary documents that support the appeal. This may include medical records, additional notes, or any correspondence related to the claim.
-
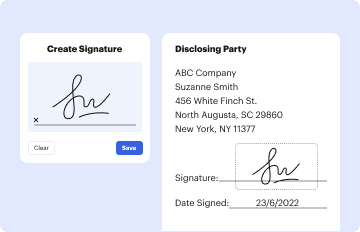
Signature:
- Ensure that the form is signed and dated by the provider or an authorized representative before submission.
Important Terms Related to the BCBS Reconsideration Form in Florida
Understanding key terms associated with the BCBS reconsideration form is beneficial for providers navigating the appeals process.
Relevant Terminology
- Claim Denial: A determination from Florida Blue stating that a claim will not be paid, often accompanied by specific reasons.
- Remittance Advice: The explanation of benefits provided by Florida Blue detailing what has been paid and what has been denied on a claim.
- Supporting Documentation: Any additional records or information that reinforce the provider's position in the appeal process.
Legal Use of the BCBS Reconsideration Form in Florida
The BCBS reconsideration form adheres to legal standards set forth for healthcare providers and insurance claims processing.
Compliance with Regulation
- ESIGN Act Compliance: Electronic submissions are recognized under the ESIGN Act, making electronically signed forms legally valid.
- Record Keeping: Providers are advised to retain copies of submitted reconsideration forms, supporting documents, and any correspondence related to the appeal process for compliance and future reference.
Filing Deadlines and Important Dates for the Reconsideration Process
Timeliness is critical when submitting the BCBS reconsideration form.
Key Deadlines
- Submission Period: Providers must submit the reconsideration form within one year from the remittance advice date for the claim in question.
- Content Review Timeline: After submission, providers can expect a response regarding the reconsideration—typically within specified timeframes set by Florida Blue.
Form Submission Methods: Online, Mail, or In-Person
Providers have multiple options for submitting the BCBS reconsideration form, allowing for flexibility in meeting their needs.
Submission Options
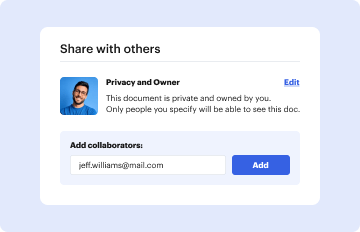
- Online: If utilizing a provider portal that allows electronic submissions, this method is often the fastest.
- Mail: Forms can be sent via postal service to the designated address indicated on the form, ensuring that they are sent within the required timeframe.
- In-Person: In specific scenarios, providers might choose to bring the form directly to a Florida Blue office; however, checking ahead for acceptance is advisable.
Examples of Using the BCBS Reconsideration Form in Florida
Practical examples can illustrate how the reconsideration form is utilized effectively by providers.
Case Studies
-
Example 1: A provider submits a reconsideration appeal for a surgery claim that was denied due to lack of prior authorization; they attach relevant correspondence and clinical notes to support the necessity of the procedure.
-
Example 2: A physician appeals for payment of a specialty consultation claim, ensuring to outline the reasoning within the form while including detailed patient records to demonstrate that the service provided was medically necessary.
These examples highlight how comprehensive documentation and a clear rationale can enhance the likelihood of a successful reconsideration.