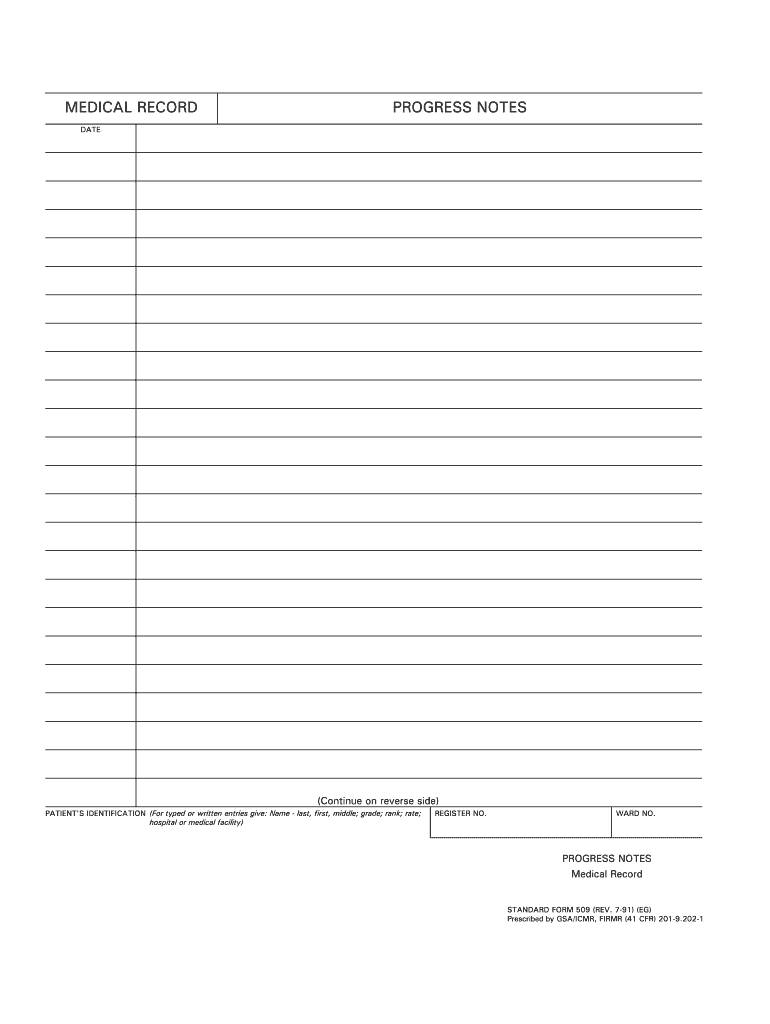
Definition and Meaning of Printable Progress Notes Template
A printable progress notes template is a structured document designed to help healthcare professionals, specifically nurses, accurately document patient observations, treatment updates, and care plans in a systematic manner. This template is an essential tool in nursing practice, serving both as a record of patient interactions and as a means of communication among medical team members.
The forms typically include various sections that cater to specific fields of information, such as patient identification details, observations, assessments, and plans for follow-up care. Utilizing a standardized template enables healthcare providers to save time, maintain accuracy, and enhance the clarity of patient records, thereby improving overall care delivery.
Progress notes are crucial in various medical fields, as they provide a legal record of patient care. This documentation is vital not only for continuity of care but also for compliance with regulatory standards. Additionally, these notes assist in reviewing treatment effectiveness and making necessary adjustments to care plans, ensuring a patient-centered approach in nursing.
How to Use the Printable Progress Notes Template
Using a printable progress notes template involves several steps that ensure efficient and effective documentation. Here is a general guide on how to utilize this template:
-
Select the Appropriate Template:
- Choose a template suited to your specific nursing practice or specialty. For example, templates may vary for pediatrics, geriatrics, or mental health.
-
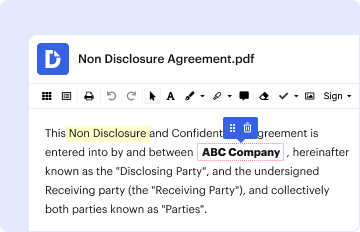
Document Patient Information:
- Fill in vital patient identification details at the top of the form, including the patient's name, date of birth, and medical record number. Include dates and times for each entry to maintain chronological accuracy.
-
Record Observations and Assessments:
- In the sections designated for observations, include key details such as vital signs, physical assessments, and any relevant patient complaints. Be specific and objective in your descriptive notes.
-
Indicate Interventions and Responses:
- Document the nursing interventions implemented and highlight patient responses to these actions. This might include changes in vital signs or patient feedback regarding pain levels or comfort.
-
Plan for Future Care:
- Utilize the template to outline future plans, including follow-up appointments, referrals, or additional treatments. Outline potential goals for patient education and involvement in their own care.
-
Review and Update:
- Consistently review and update the progress notes as additional information becomes available or circumstances change. Regular updates ensure comprehensive patient tracking.
Maintaining accurate and thorough documentation using the progress notes template improves communication within the healthcare team and promotes better patient outcomes.
Key Elements of the Printable Progress Notes Template
A comprehensive editable progress notes template typically incorporates several essential elements necessary for effective documentation. Here are key components to include:
-
Patient Identification:
- Name, date of birth, medical record number, and admission date.
-
Date and Time:
- Document the specific date and time for each entry to establish a timeline of care.
-
Subjective Data:
- Record patient's verbal statements regarding their condition, including complaints and feelings about their health status.
-
Objective Data:
- Include measurable and observable data, such as vital signs, results from physical assessments, and any diagnostic tests.
-
Assessment:
- Provide a summary of your clinical judgments based on the subjective and objective data collected.
-
Plan:
- Outline the care plan which includes interventions, treatments, and goals tailored to the patient’s needs.
-
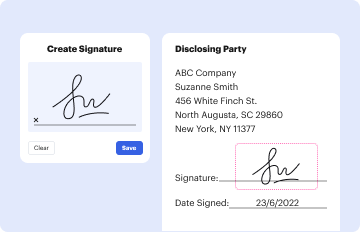
Signature and Credentials:
- Sign and date the document with your credentials to affirm the information's accuracy and completeness.
-
Space for Additional Notes:
- Consider including a section for additional remarks or critical changes in the patient's condition that may require immediate attention.
Having these elements in the progress notes template allows nurses to provide thorough documentation, fostering better communication and continuity within healthcare teams.
Who Typically Uses the Printable Progress Notes Template
Various healthcare professionals utilize a printable progress notes template, with a primary focus on nursing staff. The following groups often engage with these documents:
-
Registered Nurses (RNs):
- RNs play a critical role in patient assessment and care delivery; their documentation is vital for ongoing treatment plans.
-
Licensed Practical Nurses (LPNs):
- LPNs often assist with routine documentation and patient monitoring under the supervision of RNs.
-
Nurse Practitioners (NPs):
- NPs use progress notes to provide comprehensive patient care, reflecting their assessments and treatment plans effectively.
-
Medical Assistants:
- In some settings, medical assistants document patient interactions during routine check-ups, contributing to progress notes.
-
Health Care Administrators:
- Administrators may employ these templates to track patient progress over time, assisting with program evaluations and quality control.
-
Occupational and Physical Therapists:
- Though not nurses, these professionals document patient progress and treatment outcomes using tailored progress notes.
In summary, nursing and allied health professionals employ printable progress notes templates to ensure efficient care documentation and effective communication within multidisciplinary healthcare teams.

Important Terms Related to Printable Progress Notes Template
Understanding key terms related to progress notes templates enhances clarity and improves documentation practices in nursing. Here are essential terms to know:
-
SOAP Format:
- A widely used structure, the SOAP format stands for Subjective, Objective, Assessment, and Plan. It provides a clear and organized approach to documenting patient information.
-
Clinical Pathway:
- A clinical pathway is a predefined sequence of care for specific diagnoses, guiding healthcare providers on best practices and expected outcomes.
-
Documentation Standards:
- These are guidelines or criteria set by healthcare institutions and regulatory organizations that govern how patient information must be documented.
-
Interdisciplinary Team:
- This term refers to a group of healthcare professionals from various specialties who collaborate to provide comprehensive patient care, with documentation facilitating effective communication among team members.
-
Care Continuity:
- It refers to a consistent and seamless experience for patients as they move through different stages of care, often enhanced by thorough documentation.
Familiarity with these terms aids healthcare professionals in efficient communication and accurate patient documentation when utilizing a printable progress notes template.