Overview of Physical Therapy Documentation Templates
Physical therapy documentation templates are crucial for practitioners to manage patient records efficiently and systematically. These templates provide standardized formats that facilitate the documentation process, ensuring all vital information is captured consistently. They are especially useful for creating physical therapy progress notes, assessment documentation, and treatment plans, making them indispensable tools for therapists in acute care and outpatient settings.
Types of Physical Therapy Documentation Templates
- Assessment Templates: These templates streamline initial patient evaluations, gathering critical information regarding patient history, current conditions, and treatment goals.
- Progress Note Templates: Designed for ongoing documentation, these templates help track a patient's status, response to treatment, and any changes in their plan of care.
- SOAP Note Templates: Incorporating the Subjective, Objective, Assessment, and Plan format, SOAP notes provide a clear framework for documenting clinical findings and treatment strategies.
- Daily Note Templates: These templates are ideal for recording daily therapy sessions, including interventions used and patient responses.
Key Components of Physical Therapy Documentation
Effective documentation entails several essential components that work together to provide a complete picture of patient care:
- Patient Information: Basic demographics, medical history, and relevant social factors must be documented to understand the patient's context.
- Description of Treatment: Clear detailing of modalities, exercises, and techniques applied during therapy sessions helps ensure continuity of care and compliance with treatment protocols.
- Outcome Measures: Tracking improvements or setbacks through standardized outcome measures provides objective evidence of a patient’s progress, essential for both clinical reasoning and billing purposes.
- Plan of Care: A comprehensive plan should outline future treatment goals, frequency of visits, and any adjustments based on the patient’s ongoing evaluation.
Using Physical Therapy Documentation Templates
Documentation templates can be easily integrated into the workflow of a physical therapy practice. Here are a few steps to effectively utilize these templates:
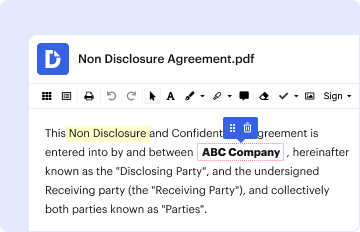
- Select the Appropriate Template: Based on the specific context or need (assessment, progress, daily notes), choose the relevant template that aligns with the intended documentation.
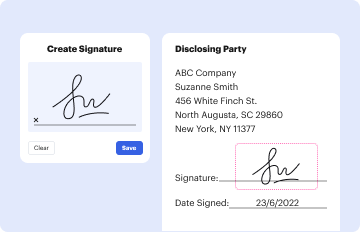
- Complete Required Fields: Fill in all necessary sections systematically, ensuring adherence to both legal and professional standards. This includes patient identifiers, date of service, and treatment duration.
- Utilize Checklists and Standardized Forms: Employ built-in checklists for pre-therapy assessments and post-therapy evaluations. This not only enhances completeness but also improves compliance during audits.
- Review and Revise: After initial completion, review the documentation for accuracy, consistency, and completeness before finalizing.
Benefits of Using Templates in Physical Therapy
Utilizing physical therapy documentation templates offers numerous advantages:
- Time Efficiency: Streamlined processes reduce the time spent on paperwork, enabling clinicians to focus more on patient care.
- Improved Compliance: Standardization encourages adherence to regulations and best practices, minimizing the risk of omissions or errors in record-keeping.
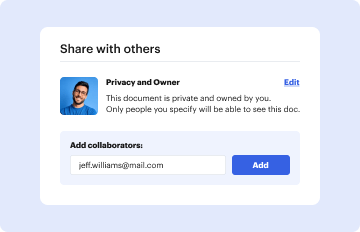
- Enhanced Communication: Well-structured documentation facilitates better communication among healthcare providers, ensuring cohesive patient management.
Real-World Scenarios for Template Use
- Outpatient Clinics: Physical therapists in outpatient settings can use documentation templates to create detailed patient records that meet the demands of insurance reimbursement and align with regulatory standards.
- Home Health Settings: Templates are equally valuable in home health scenarios where therapists must document care provided in the patient’s residence under tight time constraints.
- Acute Care Environments: In hospitals, templates enable quick and effective documentation, which is crucial when coordinating care among multidisciplinary teams.
Conclusion on Effective Documentation Practices
Implementing physical therapy documentation templates simplifies therapeutic documentation while promoting comprehensive patient care. By ensuring that all required elements are thoroughly documented, therapists can significantly enhance their practices, improve patient outcomes, and maintain compliance with professional standards. Templates serve as foundational tools that support clinicians in documenting patient interactions accurately and efficiently, ultimately benefiting both the therapist and the patient.