Definition & Meaning
The Health Insurance Premium Payment (HIPP) for Kids (HFK) Program in Virginia, often referred to as "HIPP for Kids," is a Medicaid initiative designed to help families manage the costs associated with health insurance premiums. This program targets children under the age of 19 who are eligible for Medicaid and covers them alongside their parents if they are enrolled in a qualified employer-sponsored health plan. Through this program, the state assists with cost-sharing by reimbursing eligible health insurance premiums, ensuring that families can maintain comprehensive health coverage.
Eligibility Criteria
To qualify for the HIPP for Kids Program in Virginia, applicants must meet several criteria. The child must be Medicaid-eligible and under the age of 19. Additionally, either the child or their parents should be enrolled in a qualified employer-sponsored health insurance plan. The program considers if the employer plan is cost-effective, meaning that the state's cost for assisting with the premium is less than the estimated costs for providing Medicaid services for the enrolled family members. Eligibility also requires that the health plan covers both the child and Medicaid-approved benefits.
How to Obtain the HIPP for Kids Program
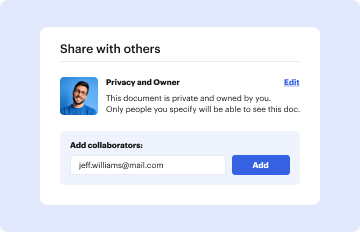
Securing access to the HIPP for Kids Program involves a series of steps. Interested families should contact the local Department of Medical Assistance Services (DMAS) office or apply online through the Virginia Medicaid portal. During the application process, proof of Medicaid eligibility for the child, documentation of enrollment in a qualifying health plan, and any pertinent financial records will be needed to assess the cost-effectiveness of participation. Following submission, the DMAS will review the application and notify the family of their enrollment status.
Required Documents
Applicants must prepare several documents to streamline their application process for the HIPP for Kids Program. Key documents include:
- Medicaid eligibility verification for the child
- Proof of enrollment in an employer-sponsored health plan
- Recent pay stubs or tax returns to verify income
- Health plan documents, such as policy details and coverage outlines
- Employer statements verifying the health plan's availability and costs
Having these documents organized and ready can expedite the application process and approval.
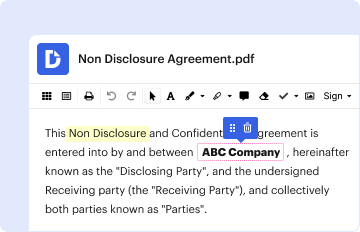
Steps to Complete the HIPP for Kids Program Application
- Gather Necessary Documentation: Collect all required documents, such as eligibility verification, income proof, and health plan details.
- Complete the Application Form: Fill out the form available on the Virginia Medicaid website or at a local DMAS office.
- Submit the Application: Provide your completed application along with the gathered documents via mail, online, or in person at a designated office.
- Follow Up with DMAS: Contact DMAS for any additional requirements or updates regarding your application status.
- Receive Confirmation and Reimbursements: Upon approval, confirmations will be sent, and premium reimbursement details will be outlined.
Key Elements of the HIPP for Kids Program
The program comprises several critical components that ensure comprehensive support for eligible families. These include:
- Cost Sharing: Reimbursement for health insurance premiums paid by the family.
- Coverage as per Medicaid Standards: Ensures that covered services align with Medicaid offerings, minimizing gaps in care.
- Renewal Requirements: Families must periodically renew their enrollment and demonstrate continued eligibility and cost-effectiveness.
State-Specific Requirements
In Virginia, the HIPP for Kids Program emphasizes state-specific mandates that dictate how the program is administered. The state's regulations require that the cost of the private or employer-sponsored health plan is less than the projected Medicaid expenses if the child received Medicaid-only services. Additionally, specific state rules govern documentation submission requirements, payment schedules for reimbursements, and compliance metrics for ongoing eligibility.
Examples of Using the HIPP for Kids Program
To better understand the pragmatic value of this program, consider the following scenarios:
-
Example 1: A family with a Medicaid-eligible child enrolled in a parent's employer health plan finds that the program reimburses them for a portion of their premium payments, reducing overall medical costs.
-
Example 2: A single parent working part-time qualifies for the HIPP for Kids Program, allowing them to maintain employer-sponsored insurance coverage for their child without facing financial hardship.
These examples illustrate how families can maintain essential health coverage through this program while alleviating financial burdens.
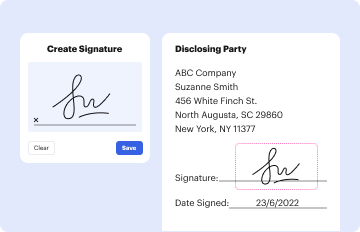
Form Submission Methods
Applicants of the HIPP for Kids Program have multiple submission options:
- Online Submission: Families can apply through the Virginia Medicaid website for faster processing.
- Mail Submission: Applications and supporting documents can be mailed to the designated DMAS office.
- In-Person Submission: Applicants may visit local DMAS offices to submit forms and receive assistance on-site.
Understanding these methods helps ensure that applications are processed efficiently and reach the appropriate channels.
Application Process & Approval Time
The application and approval process for the HIPP for Kids Program typically spans several weeks. Upon submission, the Department of Medical Assistance Services evaluates the application materials and calculates the cost-effectiveness of the family’s health plan. Approval time can vary based on completeness of documentation, volume of applications during peak periods, and any necessary follow-ups for additional information. Applicants can expect a response within four to six weeks, although processing times may be quicker for online submissions.