Definition and Purpose of eMedNY 150003
eMedNY 150003 is primarily a form used for submitting claims for Medicaid-covered services in the State of New York. The form plays a critical role in ensuring that healthcare providers can efficiently request reimbursements for services provided to Medicaid beneficiaries. By standardizing the submission process, eMedNY 150003 facilitates accurate and prompt claims processing through the eMedNY system, which is New York State’s Medicaid Management Information System. The form captures necessary details about the service rendered, the provider, and the recipient to comply with Medicaid's billing requirements.
Key Elements of the eMedNY 150003
The eMedNY 150003 form comprises various essential elements that ensure accurate data capture for claims processing.
- Provider Information: This section requires the provider’s name, address, National Provider Identifier (NPI), and contact details.
- Recipient Details: Information such as the recipient's full name, Medicaid identification number, and date of birth are needed.
- Service Information: Detailed descriptions of services provided are necessary, including dates of service, procedure codes, and charges.
- Authorization Codes: Any prior authorizations or approval codes required for particular services must be documented here.
By correctly completing these elements, providers ensure their submissions are compliant with Medicaid guidelines and decrease the likelihood of rejected claims.
How to Use the eMedNY 150003 Form
Using the eMedNY 150003 form involves a systematic approach to accurately fill out and submit claims.
- Gather Information: Collect all necessary patient and service details before starting.
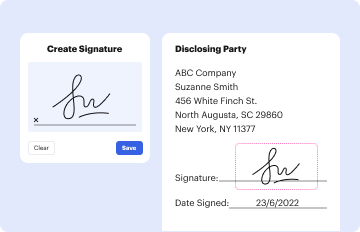
- Complete Form Sections: Accurately fill in each section as discussed in key elements.
- Review for Accuracy: Double-check all entries to prevent errors that could lead to claim denials.
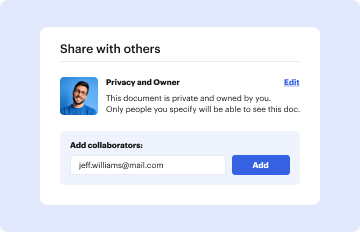
- Submit Form: Utilize the appropriate submission method, either electronically through the eMedNY system or via post, ensuring forms are submitted in accordance with New York Medicaid requirements.
Obtaining the eMedNY 150003 Form
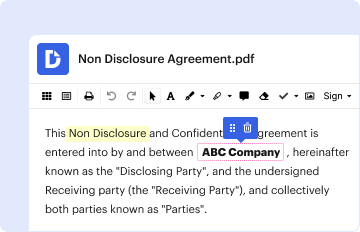
To obtain the eMedNY 150003, providers can access it through the eMedNY website where downloadable versions are available.
- Online Access: The eMedNY portal provides a comprehensive platform for downloading necessary forms, including 150003, in PDF format.
- In-Person Requests: Providers can also contact local Medicaid offices for physical copies if required.
Having easy access to this form ensures providers can consistently meet their billing obligations.
Steps to Complete the eMedNY 150003
Completing the eMedNY 150003 requires attention to detail to avoid claim errors.
- Provider Details Entry: Fill out provider business details and identifiers.
- Input Recipient Information: Enter patient-specific details related to Medicaid eligibility.
- Accurately Document Services: List each service provided along with specific codes and dates.
- Include Authorization Codes: If services require pre-approval, ensure codes are included and correct.
- Conduct a Thorough Check: Before submission, review the entire form for completion and accuracy of data.
Importance of eMedNY 150003 for Providers
The eMedNY 150003 form is vital for healthcare providers participating in New York's Medicaid program. It ensures:
- Timely Reimbursements: Proper and timely completion leads to efficient processing and reimbursement of claims.
- Compliance with Guidelines: Adheres to state-specific Medicaid billing guidelines, minimizing the risk of errors and penalties.
- Streamlined Process: Contributes to a streamlined billing and payment process for services rendered to Medicaid recipients.
Legal Use and Compliance Regarding eMedNY 150003
Compliance with legal guidelines is imperative when using the eMedNY 150003. Providers must adhere to HIPAA regulations, ensuring patient information privacy and security. Additionally:
- Documentation Accuracy: Maintain honest and accurate records of services provided.
- Authorization Compliance: Ensure all services requiring pre-approval are documented with corresponding authorization numbers.
Non-compliance can lead to penalties and claim denials, necessitating strict adherence to Medicaid guidelines.
Examples of Using eMedNY 150003 in Practice
In practical scenarios, the eMedNY 150003 is used for submitting claims related to a variety of healthcare services. For instance:
- Routine Check-Ups: Physicians submit claims for general medical services, noting the routine care specific codes.
- Specialist Consultations: Specialists bill for advanced procedures such as diagnostics by including relevant procedure and diagnosis codes.
- Emergency Services: Hospitals ensure quick documentation submission for emergency medical interventions to guarantee prompt reimbursements.
These examples underline the eMedNY 150003 form's role in facilitating diverse healthcare claims under Medicaid.