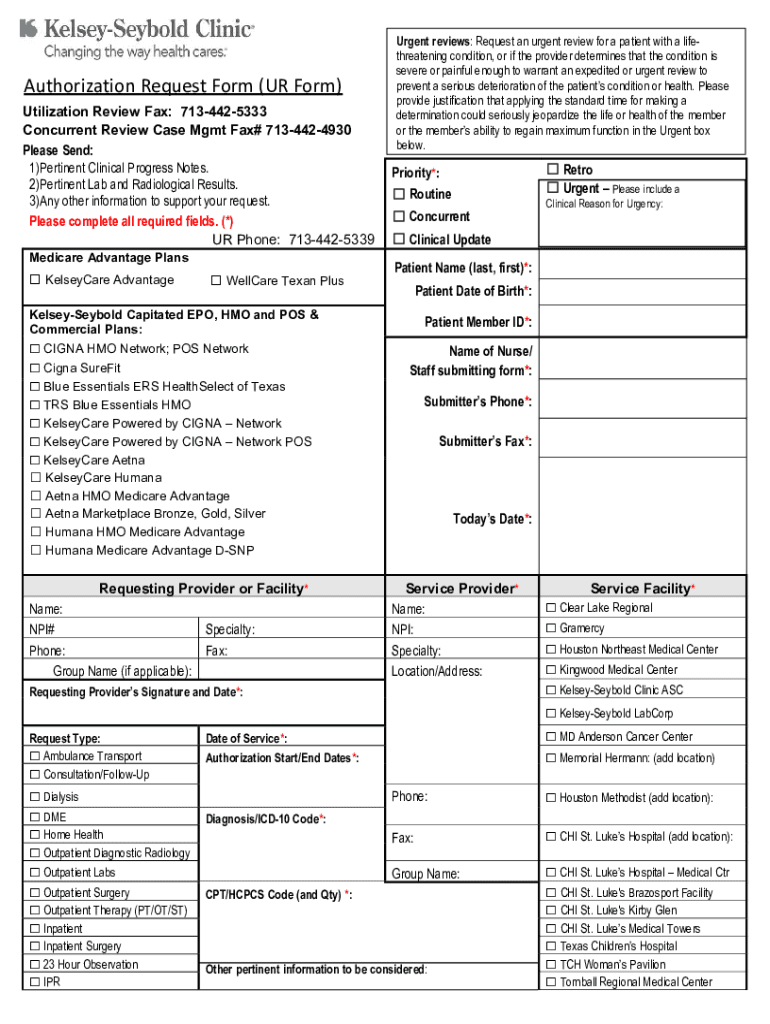
Definition and Meaning of the Authorization Request Form (UR Form)
The Authorization Request Form, commonly referred to as the UR Form, is an essential document used within healthcare systems to streamline the process of utilization review. This form is primarily used by medical professionals, insurance providers, and patients to request authorization for specific medical services and treatments under managed care plans. Such forms are critical for ensuring that services meet the criteria established by healthcare providers and insurance companies, thus preventing unnecessary procedures and facilitating efficient use of resources.
The UR Form outlines various sections that capture pertinent information, including patient identification data, details of the service requested, and clinical justification for the service. By having these details clearly articulated, the form aids in making informed decisions regarding the authorization of medical procedures, medications, or therapy sessions.
Steps to Complete the Authorization Request Form (UR Form)
-
Gather Necessary Information: Ensure you have all the required details at hand, such as patient information, insurance provider details, and the medical necessity of the requested service.
-
Patient Details Section: Begin by accurately filling out the patient’s name, ID number, and contact information. This section is crucial for identifying which individual the authorization request pertains to.
-
Clinical Justification: A comprehensive explanation of why the requested service or procedure is necessary. Include any supporting documents, such as medical records or previous treatment attempts, that can substantiate the request.
-
Service Provider Information: Input the details of the healthcare provider or facility that will render the service. This includes names, contact information, and any pertinent provider identifiers.
-
Type of Request: Specify if the review is urgent or routine. Urgent requests typically have expedited processes, ensuring timely access to necessary treatments.
-
Submission of Form: Once all sections are completed, double-check for accuracy. Submit via the designated method, whether online, by mail, or in person, as stipulated by the insurance provider.
How to Use the Authorization Request Form (UR Form)
Understanding how to effectively use the UR Form can greatly impact the approval process of medical services. Primarily, this form is used to present a formal request for reviewing and authorizing healthcare services under a particular insurance policy. Users need to be meticulous in how they fill out and submit this form, as any discrepancies can delay the review process.
The UR Form acts as a bridge between the healthcare provider and the insurance company, facilitating communication about what medical services are needed and why they are justified. It's a key component of patient advocacy as well, as all necessary information must be presented clearly and convincingly to secure the required approvals without undue delay.
Reasons to Use the Authorization Request Form (UR Form)
-
Ensure Compliance: Utilizing the UR Form ensures that all necessary medical services follow the proper regulatory guidelines and insurance policy requirements, minimizing the risk of service denial.
-
Streamline Authorization Process: By compiling all relevant patient and service information into a standardized form, healthcare providers can efficiently manage and track authorization requests.
-
Prevent Unnecessary Services: By requiring detailed justification, the UR Form helps prevent unnecessary medical procedures, thereby optimizing resource utilization within healthcare facilities.
-
Facilitate Patient Care: Timely authorization of necessary medical services ensures that patients receive the appropriate care without undue delay or financial burden.
Important Terms Related to the Authorization Request Form (UR Form)
Understanding specific terminology related to the UR Form is crucial for its correct application:
-
Utilization Review (UR): A process by which healthcare services are reviewed for their necessity, efficiency, and appropriateness.
-
Clinical Justification: Detailed reasoning for why a medical service is needed, often including patient symptoms, diagnosis, and how the service will address these issues.
-
Prior Authorization: An insurance plan requirement that certain medical services be pre-approved following a submission and review of the UR Form.
-
Urgent vs. Routine Requests: Differentiation between services that require rapid approval due to their immediate necessity versus those that can undergo standard review timelines.
Key Elements of the Authorization Request Form (UR Form)
-
Patient Identification Information: Basic details that link the form to the specific patient needing the services.
-
Medical Service or Procedure Description: Concisely describes the treatment or service proposed.
-
Clinical Justification and Documentation: Supports the necessity of the requested procedures with relevant patient history and medical assessments.
-
Insurance Information: Includes details of the patient's insurance policy and the scope of covered services, ensuring correct billing and approval processes.
Examples of Using the Authorization Request Form (UR Form)
A practical example of using the UR Form includes a scenario where a physician requests an MRI for a patient who has been experiencing unexplained neurological symptoms. The form will detail the symptoms, previous diagnoses, and why an MRI is the most appropriate next step for diagnosis. Another example involves a patient requiring surgery for a complex fracture; the form would include X-ray results, the surgical plan, and projected outcomes to justify the surgery request.
By understanding these examples, users can better appreciate how to fill out and submit the UR Form effectively to secure the necessary health services upon which effective treatment hinges.