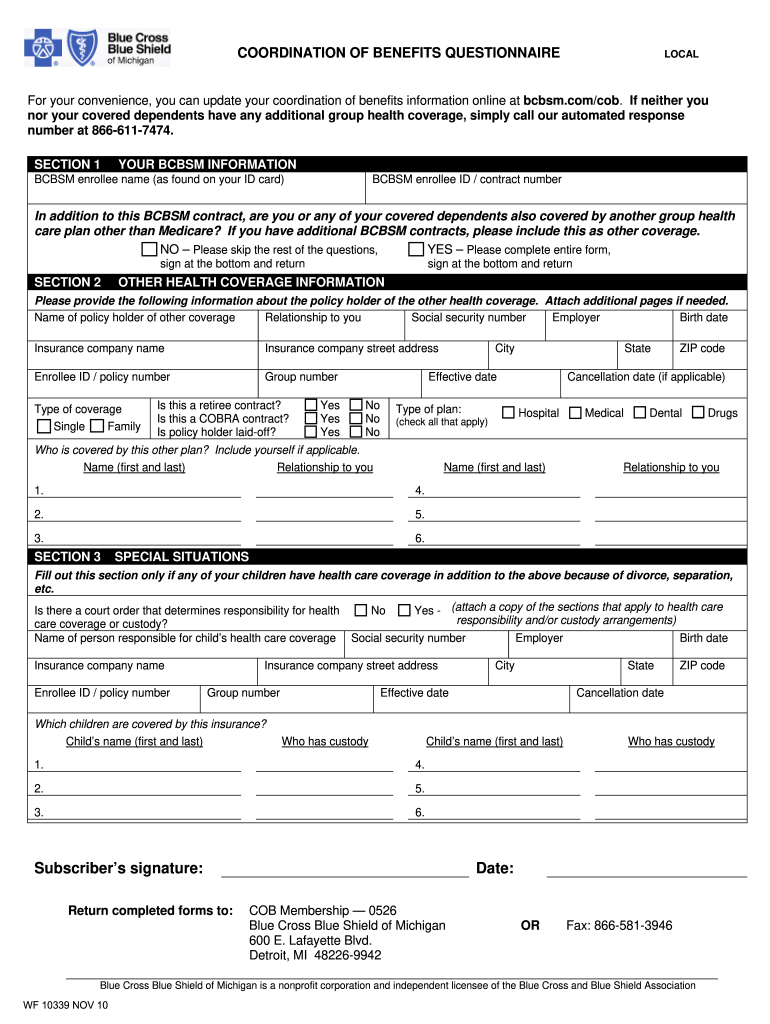
Definition & Meaning of the Coordination Benefits Form
The coordination benefits form is a document used primarily to collect information about an individual's or family's additional health coverages. This form plays a crucial role in coordinating benefits among multiple insurance providers, ensuring that claims can be processed effectively and without duplication. By gathering details about all active health insurance policies, including those held by dependents, the form aids in determining which insurance will be the primary payer for medical services.
- Purpose of the Form: The coordination benefits form is essential for health insurance companies to process claims efficiently, thereby reducing the risk of incorrect payments and potential fraud.
- Impact on Coverage: Accurate information submitted can enhance coverage management, as it helps insurance companies align services and payments based on the policyholder's overall health insurance status.
Steps to Complete the Coordination Benefits Form
Filling out the coordination benefits form requires specific information that must be gathered accurately. Following a systematic approach ensures all necessary details are included.
- Gather Personal Information: Collect data related to the individuals covered under the insurance policy. This typically includes names, dates of birth, and relationship to the primary policyholder.
- List All Insurance Policies: Document all health insurance plans in which the individual or dependents are enrolled. Include the name of the insurance company, policy numbers, and coverage type.
- Provide Details on Coverage: Specify the nature of the coverage, including whether it is through an employer, a government program, or a private plan. Include effective dates and cancellation dates if applicable.
- Highlight Special Situations: If there are unique circumstances, such as custody arrangements for dependents, these should be clearly noted to avoid any confusion in the claims process.
- Review and Submit: Before sending the form, review all entries for accuracy to ensure no information is missing or incorrect.
How to Obtain the Coordination Benefits Form
Obtaining the coordination benefits form can be achieved through various avenues to accommodate different preferences.
- Insurance Providers: Most insurance companies provide this form via their websites or through customer service representatives. Checking the relevant health insurance company’s website or calling their help line can yield quick results.
- National Insurance Associations: Organizations such as the National Association of Insurance Commissioners may offer downloadable versions of the coordination benefits form.
- Healthcare Facilities: Hospitals and clinics may also provide this form during appointments or visits, particularly when there is a need for insurance processing.
Important Terms Related to the Coordination Benefits Form
To fully understand the coordination benefits form, familiarity with specific terminology can be beneficial:
- Primary Payer: The insurance plan that pays first, covering eligible medical expenses before any other insurance applies.
- Secondary Payer: The additional insurance policy that will pay after the primary payer has processed a claim.
- Coverage Type: This refers to the kind of health care services offered by an insurance plan, such as comprehensive, major medical, or limited benefits.
- Dependent: Individuals covered under someone else's insurance policy, such as children or spouses.
These terms are vital for accurately filling out the coordination benefits form and for ensuring effective communication with insurance representatives.
Why You Should Use the Coordination Benefits Form
Utilizing the coordination benefits form offers several advantages for policyholders and their dependents:
- Maximizes Benefits: Ensures that all applicable health insurance benefits are utilized, leading to lower out-of-pocket costs for medical services.
- Reduces Claim Denials: By clearly identifying all sources of coverage, this form can help minimize the chances of claim denials due to overlooked insurance policies.
- Streamlines Medical Billing: Assists healthcare providers in efficiently coordinating payments between different insurers, speeding up the billing process and improving patient experiences.
Understanding the benefits of this form is essential for anyone navigating multiple health insurance plans.