Definition & Meaning
The Admission Concurrent Review Fax Form serves as a critical tool in the healthcare industry, mainly focusing on the efficient tracking of patient admissions and discharges. This document outlines the necessary information for managing patient transitions between healthcare services and facilities. It is designed to facilitate the communication process among healthcare providers, ensuring that all relevant parties are informed about patient status changes to ensure continuity of care. Fields typically include patient demographics, reason for admission, expected length of stay, and initial diagnosis codes.
How to Use the Admission Concurrent Review Fax Form
Using the Admission Concurrent Review Fax Form involves a series of steps to ensure accurate and complete information transmission:
- Complete Patient Details: Begin by entering the patient's personal information, including name, date of birth, and medical record number.
- Fill Admission Type: Specify the type of admission—emergency, elective, or referral. This classification helps prioritize care.
- Outline Diagnosis Codes: Use the provided space to enter initial diagnosis codes using standardized medical classifications to ensure clarity.
- Include Admission Dates: List the admission and expected discharge dates to track patient stay duration.
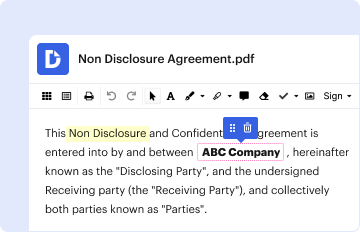
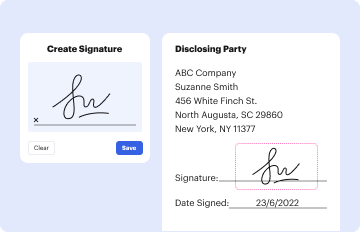
- Sign and Date: Ensure the form is signed by an authorized healthcare provider and dated to authenticate the document.
Steps to Complete the Admission Concurrent Review Fax Form
Completing the Admission Concurrent Review Fax Form requires attention to detail to minimize errors:
- Gather Necessary Information: Before beginning, collect all necessary patient information, including medical history and current treatment plans.
- Check for Accuracy: As you fill out the form, double-check entries for accuracy, especially diagnosis codes and patient identifiers.
- Attach Supporting Records: Include any relevant medical records or previous consultation notes that provide context for the admission.
- Review Form Comprehensively: Ensure that all sections are filled correctly and that no required fields are left blank.
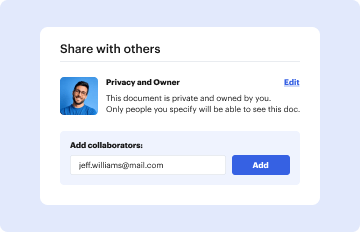
- Send through Approved Channels: Once completed, fax the form using secure, authorized channels to maintain confidentiality.
Key Elements of the Admission Concurrent Review Fax Form
Several key elements must be consistently present on the Admission Concurrent Review Fax Form:
- Patient Identification Information: Accurate identification details such as full name, date of birth, and patient ID are crucial for correctly logging and tracking.
- Admission Details: Specifics about the type and reason for admission and required services to provide appropriate care.
- Medical Codes and Diagnoses: Standardized codes must be used to avoid miscommunication.
- Confidentiality Notifications: Detailed information about how the patient's information will be protected are typically included.
- Authorization Section: Space for signatures to indicate form approval and data verification.
Legal Use of the Admission Concurrent Review Fax Form
The legal use of the Admission Concurrent Review Fax Form is governed by healthcare laws and regulations that protect patient information and ensure proper documentation:
- HIPAA Compliance: The form must comply with the Health Insurance Portability and Accountability Act (HIPAA) to protect sensitive patient health information.
- Informed Consent: Patients or their legal guardians must be aware that their information will be used for healthcare coordination.
- Record Keeping: Correctly filled forms become part of the patient's legal medical record and must be stored appropriately according to legal requirements.
Important Terms Related to Admission Concurrent Review Fax Form
Understanding important terms and terminology related to the Admission Concurrent Review Fax Form is vital:
- Concurrent Review: Ongoing assessment of a patient's care during their stay to ensure the appropriate allocation of resources.
- Diagnosis Codes: International Classification of Diseases (ICD) codes or equivalent standards used for medical classification.
- Admission Status: The condition under which a patient is admitted, indicating urgency and reason for service.
- PHI (Protected Health Information): Information protected under HIPAA that must be handled with strict confidentiality.
Required Documents for the Admission Concurrent Review Fax Form
Several documents are necessary when preparing the Admission Concurrent Review Fax Form:
- Patient Identification: Driver's license or official ID for verification.
- Medical Records: Previous and current medical records supporting the reason for admission.
- Insurance Information: Active insurance details to plan for coverage and billing.
- Healthcare Proxy or Guardianship Papers: If applicable, to prove the authority of the person completing the form.
Form Submission Methods
The form can be submitted through several methods, each with specific considerations:
- Fax: A direct and secure method, especially when facilities have designated secure fax lines.
- Mail: Can be used where digital submission isn't possible, though it's slower and less secure.
- In-Person: Direct handover to the admitting office or appropriate department, ensuring secure transfer.
Using secure and approved methods is crucial to protect patient privacy and ensure timely processing. Each institution may have preferences based on resources and digital infrastructure.