Understanding the mi bcbs appeal
The mi bcbs appeal, or Michigan Blue Cross Blue Shield appeal, is a formal request made by healthcare providers or insured members to challenge decisions made by Blue Cross Blue Shield of Michigan regarding claims or clinical editing denials. Understanding this appeal process is crucial for providers and members seeking adjustments or clarifications on coverage or claim outcomes.
Purpose of the mi bcbs appeal
The primary goal of the mi bcbs appeal is to provide a structured way to contest decisions that deny payment or coverage for services rendered. The appeal can address various issues, including but not limited to:
- Clinical editing denials, where a service is not approved based on coding or medical necessity.
- Payment discrepancies, such as underpayments or denials based on network status.
- Coverage issues, where services are deemed not eligible under the patient's plan.
Typical Users of the mi bcbs appeal
Both providers and members commonly use the mi bcbs appeal. Understanding who typically engages in this process can help in refining the approach:
- Healthcare Providers: Physicians, clinics, and hospitals initiate appeals to recover costs related to services they have provided that were denied or underpaid.
- Members: Insured individuals may appeal on their own behalf to contest decisions affecting their coverage for specific treatments or procedures, ensuring they receive the benefits entitled under their policy.
Important terms associated with the mi bcbs appeal
Familiarity with key terminology can enhance understanding of the mi bcbs appeal process. Important terms include:
- Clinical Editing: The process by which BCBS reviews claims for compliance with coding standards and medical necessity guidelines.
- Denial Codes: Specific codes provided by the insurer that explain the reason for a denial, critical for the appeal process.
- Supporting Documentation: Additional materials that may be required during the appeal process, such as medical records or notes.
Steps to Complete the mi bcbs appeal
Completing the mi bcbs appeal involves several precise steps to effectively challenge a denial. The process typically includes:
-
Review the Denial: Start by carefully reviewing the denial letter issued by BCBS. Pay close attention to the denial codes and reasons for denial, which will guide your appeal.
-
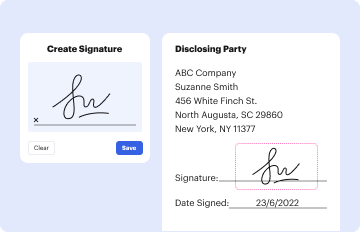
Gather Required Documents: Collect all necessary supporting documents, including patient records, previous claims submitted, and any other relevant information that substantiates the appeal.
-
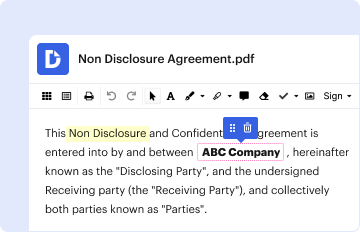
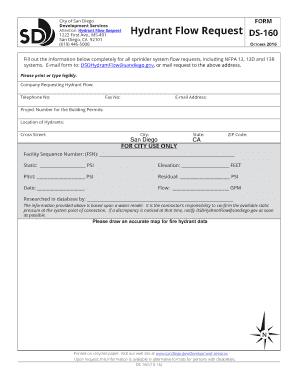
Complete the Appeal Form: Fill out the mi bcbs appeal form or relevant clinical editing appeal form carefully. Ensure that all sections are accurately completed, including:
- Provider and member details
- Procedure codes and service dates
- A clear explanation of why the denial should be overturned.
-
Submit the Appeal: Choose your submission method. Appeals can often be sent via:
- Mail: Ensure that all documents are securely bound and sent to the correct address.
- Fax: If preferred, appeals can be faxed to the claims department.
- Online Submission: Some providers may have the option to upload appeals directly through their BCBS portal.
-
Monitor Appeal Status: After submission, track the status of your appeal. It’s important to follow up if you do not receive confirmation or a response within a reasonable timeframe.
Required Documents for the mi bcbs appeal
When preparing to file the mi bcbs appeal, several documents are often required to support the claim. These include:
- Medical records relevant to the case
- Referral letters or notes
- Prior Authorization documents, if applicable
- A copy of the denial notice detailing the reasons for denial
- Any other documentation that can strengthen the case, such as clinical guidelines or research supporting the medical necessity of the service.
Submission Methods for the mi bcbs appeal
Submitting the mi bcbs appeal can be done through various channels to ensure the process is as efficient as possible:
-
Online Portal: Many providers can submit appeals directly through the BCBS online portal, which often expedites review and response times. This method is typically preferred for its convenience and tracking capabilities.
-
Mail: Sending an appeal via mail requires proper addressing and includes all necessary documents. Use a reliable mailing service to ensure that the documents are received.
-
Fax: Faxing appeals may be secure and fast, but confirmation of receipt is essential to ensure the appeal was submitted correctly.
Legal Aspects of the mi bcbs appeal
Understanding the legal implications surrounding the mi bcbs appeal is critical for both providers and members.
-
Timeliness: Appeals typically must be submitted within 180 days of the original denial, adhering to the contractual and legal timeframes set forth in provider agreements or member contracts.
-
Legally Binding Outcomes: Decisions made following an appeal are binding, so adherence to submission guidelines and accuracy in documentation is paramount.
-
State Regulations: The mi bcbs appeal process must comply with Michigan state laws governing insurance and healthcare, ensuring all legal standards are met during the appeals process.
Conclusion on mi bcbs appeal
The mi bcbs appeal process serves a critical function in the healthcare system, allowing for redress in cases where claims or coverage for services are denied. Understanding the purpose, procedures, and legal context surrounding this appeal helps both members and providers navigate the complexities of healthcare appeals successfully, ensuring that patients receive the care they need and providers are compensated fairly for their services.