Definition and Meaning of the Health Insurance Claim Form
A health insurance claim form is a standardized document used by healthcare providers to submit requests for payment or reimbursement from insurance companies for services rendered to patients. This form is crucial in the healthcare billing process, ensuring that both providers and insurers maintain accurate records of the services provided, the costs associated, and the appropriate coverage under a patient's health plan.
The most commonly used form in the United States is the CMS-1500 form. This form is used by non-institutional providers, such as physicians and independent practitioners, to claim reimbursements for medical services. Each section of the claim form is designed to capture specific information needed for processing and determining the amount owed by the insurance company. Understanding each part of the claim form is essential for accurate billing and timely reimbursements.
Health insurance claim forms also include essential terms and codes, such as procedure codes and diagnosis codes, which correspond to the services provided and the medical conditions treated. This detail helps insurers assess the legitimacy and necessity of the claimed amount, streamlining the reimbursement process and minimizing delays.
Key Elements of the Health Insurance Claim Form
The health insurance claim form is composed of various sections, each serving a distinct purpose. Here are the key elements typically found in a health insurance claim form:
-
Patient Information: This section includes the patient's name, address, date of birth, and insurance policy details. Accurate patient information is critical for linking claims to the correct insurance account.
-
Provider Information: Providers fill in their details, including name, NPI (National Provider Identifier), and contact information. This identification is essential for insurance companies to verify the credentials of the billing entity.
-
Service Information: This portion specifies the services provided, including procedure codes (CPT or HCPCS codes) and corresponding diagnosis codes (ICD codes). Each code categorizes the nature of the visit or treatment.
-
Date of Service: The claim form requires the date(s) on which services were provided. This is crucial for insurance verification and validation.
-
Charges: Total charges for each service rendered need to be itemized and clearly stated to allow for precise calculations during the reimbursement process.
-
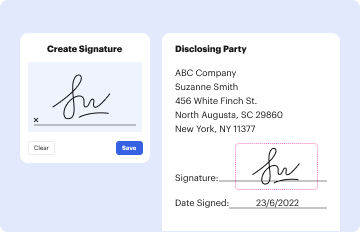
Signature: A patient or authorized representative usually signs the form to authorize the release of the information necessary for claims processing, confirming that they consent to the billing and any subsequent obligations.
Understanding these elements is important as they ensure that the claim is filled out correctly to prevent processing delays or denials from the insurance company.
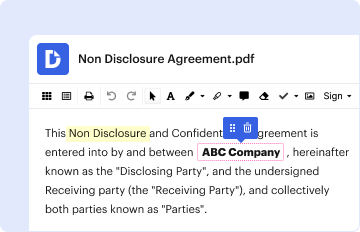
Steps to Complete the Health Insurance Claim Form
Filling out a health insurance claim form requires careful attention to detail to ensure accuracy and completeness. Here are the steps involved in completing the form:
-
Gather Necessary Information: Before you begin filling out the form, collect all required documents, including the patient’s insurance card, any pre-authorization forms, and relevant medical records.
-
Complete Patient Information: Fill in the patient's demographic details such as name, address, date of birth, and insurance policy number. Make sure this information exactly matches what is on the insurance card to avoid miscommunication.
-
Enter Provider Information: Include the provider’s name, address, and NPI number. This identification must be accurate and match the records held by the insurance company.
-
List the Services Provided: For each service, include the date of service, procedure codes, and the total charges. Be thorough in detailing each service, as errors here can lead to claim denials.
-
Check for Required Signatures: Ensure that the patient or their legal representative has signed the authorization section of the claim form. This signature is necessary for the release of their medical information for billing purposes.
-
Review and Submit: Review the completed claim form for accuracy before submission. Ensure that all fields are filled out appropriately and legibly. Submit the claim as directed by the insurance provider—either electronically or via mail.
Following these steps meticulously can help prevent common pitfalls and errors that can delay claim processing.
Important Terms Related to the Health Insurance Claim Form
Understanding the terminology associated with health insurance claim forms is essential for both patients and providers. Here are some important terms to be familiar with:
-
CPT Codes: Current Procedural Terminology codes are used to describe medical services and procedures performed by healthcare providers.
-
ICD Codes: International Classification of Diseases codes are diagnostic codes that represent the diagnosis made during the patient's visit. These codes are critical for claims approval.
-
NPI: The National Provider Identifier is a unique identification number for healthcare providers issued by the Centers for Medicare & Medicaid Services. It is mandatory for submitting claims.
-
Deductible: The amount a patient must pay for their healthcare services before the insurance company starts to pay its share.
-
Coinsurance: A cost-sharing arrangement in which the patient pays a percentage of the costs of covered healthcare services after a deductible is met.
These terms are fundamental in navigating the health insurance claim process and understanding the various aspects of healthcare billing.
Examples of Using the Health Insurance Claim Form
Practical examples can demonstrate how to effectively utilize the health insurance claim form in various scenarios. Here are a couple of common situations:
-
Example 1: Routine Medical Visit
- A patient visits a primary care physician for a routine check-up and has services rendered, including a physical examination and diagnostic blood work. The provider fills out the CMS-1500 form by including the pertinent details in the patient and provider sections, documenting the services rendered with corresponding CPT and ICD codes, and submits the claim, expecting reimbursement based on their insurance policy's coverage terms.
-
Example 2: Specialist Referral
- A patient is referred to a specialist for knee surgery. Before the appointment, they ensure that the specialist is in-network. After the surgery, the specialist submits a claim using the CMS-1500 form that lists all services provided, including pre-operative consultations and post-operative follow-ups. The claim is processed by the insurance company, facilitating the reimbursement process with adherence to the referral guidelines outlined in the patient's insurance policy.
These examples showcase the form's application across different healthcare settings, emphasizing its importance in securing payment for services rendered. Each example illustrates the need for careful and precise documentation to facilitate smooth transactions between providers and insurance companies.