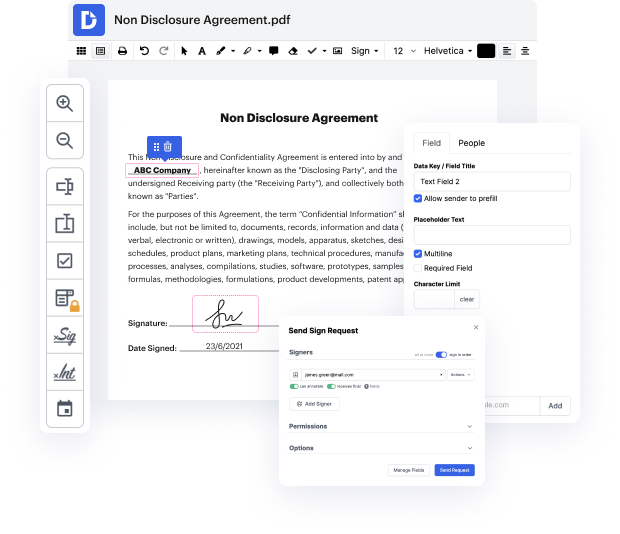
Getting comprehensive control over your documents at any moment is vital to alleviate your daily tasks and boost your productivity. Accomplish any goal with DocHub features for papers management and convenient PDF file editing. Gain access, adjust and save and integrate your workflows along with other protected cloud storage.
DocHub gives you lossless editing, the possibility to use any format, and securely eSign papers without having looking for a third-party eSignature option. Get the most of the file managing solutions in one place. Check out all DocHub features right now with your free profile.
In this tutorial, the speaker from Osmosis discusses how to write effective progress or clinical notes using the SOAP format. SOAP stands for Subjective, Objective, Assessment, and Plan. Subjective refers to the patient's statements, Objective includes findings from physical exams or tests, Assessment is the clinician's evaluation of the patient, and Plan outlines the next steps in treatment. The speaker intends to provide three key tips for crafting a good SOAP note, emphasizing the format's universal use in clinical settings.
At DocHub, your data security is our priority. We follow HIPAA, SOC2, GDPR, and other standards, so you can work on your documents with confidence.
Learn more



