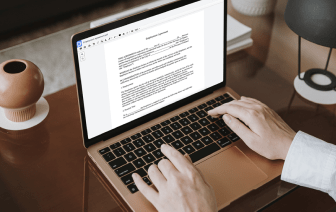
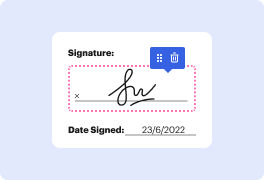
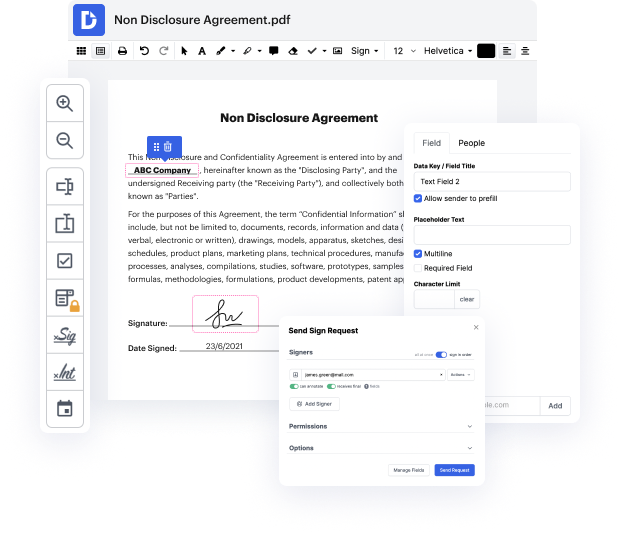
Time is a crucial resource that every enterprise treasures and attempts to convert in a gain. When selecting document management software program, take note of a clutterless and user-friendly interface that empowers customers. DocHub gives cutting-edge features to enhance your document management and transforms your PDF editing into a matter of a single click. Replace Date from the Soap Note with DocHub in order to save a lot of time as well as improve your productivity.
Make PDF editing an easy and intuitive operation that helps save you plenty of valuable time. Quickly change your files and send them for signing without the need of looking at third-party software. Focus on pertinent duties and improve your document management with DocHub starting today.
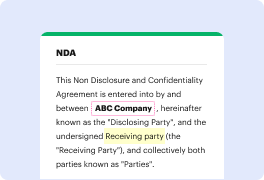
In this tutorial, the speaker discusses how to write an effective clinical or progress note using the SOAP format, which stands for Subjective, Objective, Assessment, and Plan. The subjective section contains patient-reported information, while the objective section includes the clinician's findings from physical exams, labs, or imaging. The assessment reflects the clinician's thought process and diagnosis, and the plan outlines the next steps for patient care. The speaker shares three key tips for writing a good note, emphasizing the importance of clarity and organization in the documentation process.