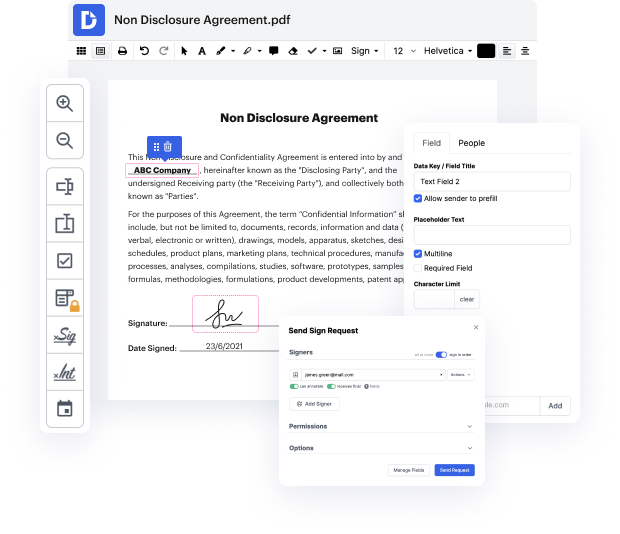
Getting complete power over your documents at any moment is vital to ease your day-to-day tasks and boost your productivity. Achieve any goal with DocHub tools for papers management and practical PDF file editing. Gain access, change and save and integrate your workflows along with other safe cloud storage services.
DocHub offers you lossless editing, the chance to work with any formatting, and safely eSign papers without the need of searching for a third-party eSignature software. Get the most of the document managing solutions in one place. Try out all DocHub functions right now with your free account.
In this video, Dr. Decide from Osmosis discusses how to write an effective clinical or progress note, particularly using the SOAP format. SOAP stands for Subjective, Objective, Assessment, and Plan. The Subjective section includes what the patient reports, the Objective part encompasses findings from the exam or tests, the Assessment outlines the clinician's understanding of the situation, and the Plan details the next steps for treatment. Dr. Decide emphasizes the importance of this format as a universal guideline and shares three top tips for writing a strong note, aiming to enhance clarity and comprehensiveness in clinical documentation.
At DocHub, your data security is our priority. We follow HIPAA, SOC2, GDPR, and other standards, so you can work on your documents with confidence.
Learn more



