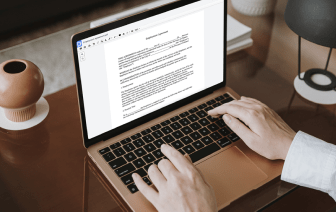
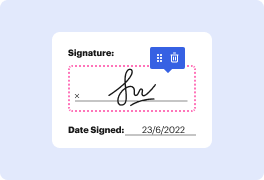
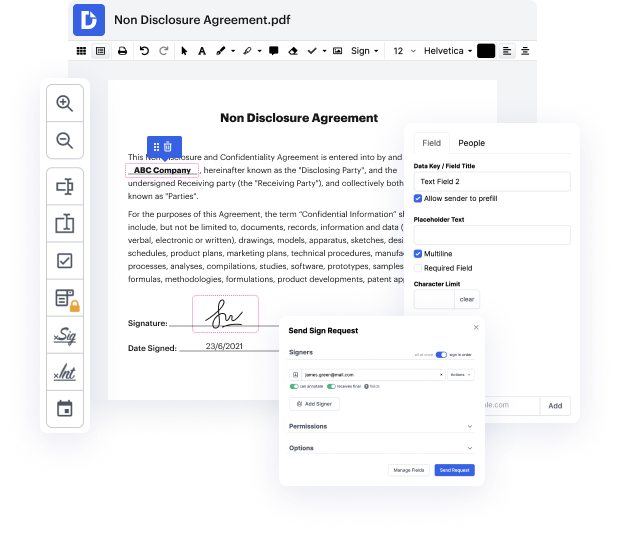
Handling and executing documents can be cumbersome, but it doesn’t have to be. No matter if you need assistance daily or only sometimes, DocHub is here to supply your document-centered tasks with an extra efficiency boost. Edit, leave notes, complete, sign, and collaborate on your Patient Progress Report rapidly and easily. You can modify text and images, build forms from scratch or pre-made templates, and add eSignatures. Due to our top-notch safety precautions, all your data remains safe and encrypted.
DocHub offers a complete set of capabilities to streamline your paper processes. You can use our solution on multiple platforms to access your documents wherever and anytime. Enhance your editing experience and save time of handiwork with DocHub. Try it for free today!
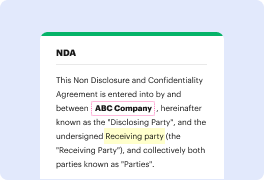
In this video, the speaker from Osmosis discusses how to write an effective progress or clinical note, focusing on the SOAP (Subjective, Objective, Assessment, Plan) format. The Subjective section captures what the patient reports, while the Objective section includes findings from physical exams, labs, or imaging. Assessment involves the clinician's reasoning about the patient’s condition, and the Plan outlines the next steps for treatment. The speaker emphasizes the universality of the SOAP format and intends to share three key tips for writing a comprehensive and effective note.