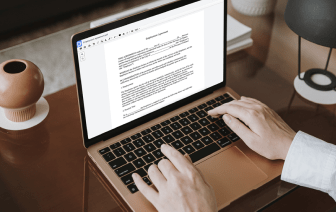
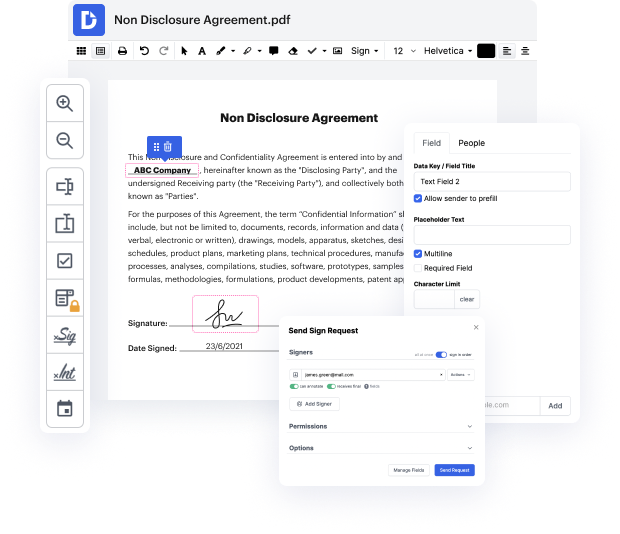
Getting comprehensive power over your documents at any moment is crucial to alleviate your day-to-day duties and improve your efficiency. Achieve any objective with DocHub tools for papers management and practical PDF file editing. Gain access, change and save and integrate your workflows with other protected cloud storage services.
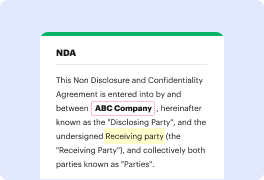
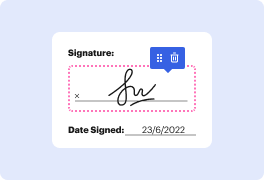
DocHub offers you lossless editing, the possibility to use any format, and securely eSign papers without having searching for a third-party eSignature alternative. Maximum benefit from the file management solutions in one place. Check out all DocHub capabilities right now with the free account.
This video tutorial covers the SOAP progress notes, a documentation method used by nurses and healthcare providers for patient charting. SOAP stands for subjective, objective, assessment, and plan. The "S" refers to subjective information, which captures what the patient reports about their experiences, including their complaints and concerns in their own words. For instance, patients might express feelings like "achy all over" or describe symptoms like a sore throat. This section should detail onset, location, frequency, intensity, duration, and factors that alleviate or exacerbate the symptoms. Additionally, when seeing a patient for the first time, it's important to include their medical, surgical, family, and social history, as well as current medications.