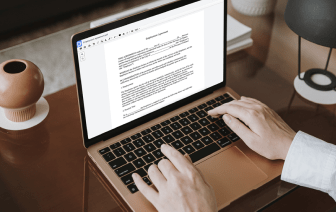
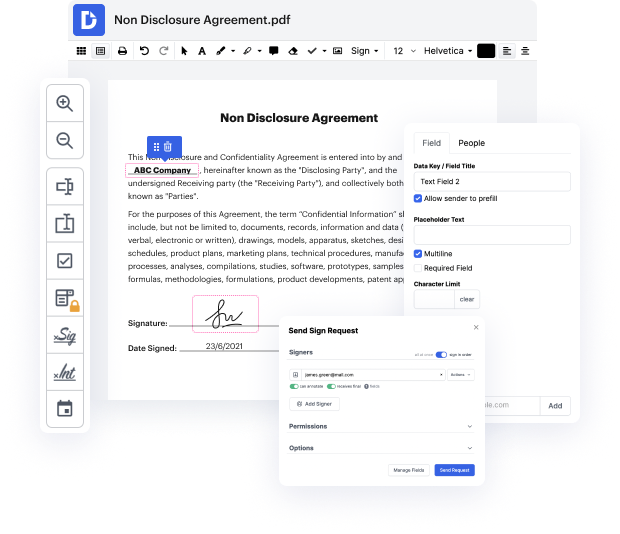
Having complete control of your documents at any moment is essential to relieve your day-to-day tasks and enhance your efficiency. Achieve any objective with DocHub tools for papers management and convenient PDF editing. Gain access, adjust and save and integrate your workflows along with other secure cloud storage.
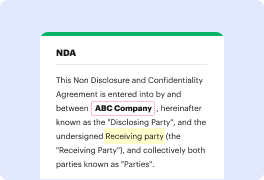
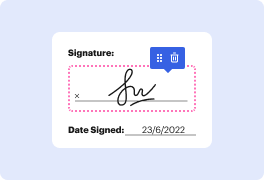
DocHub gives you lossless editing, the possibility to use any formatting, and securely eSign documents without looking for a third-party eSignature software. Make the most from the document managing solutions in one place. Consider all DocHub capabilities today with the free of charge profile.
This video tutorial covers SOAP progress notes, a documentation method used by nurses and healthcare providers. SOAP stands for Subjective, Objective, Assessment, and Plan. The Subjective component involves the patient's own words about their experiences and feelings, including complaints and concerns. It details the onset, location, frequency, intensity, duration, and factors that alleviate or worsen their condition. For new patients, it is essential to include medical, surgical, family, and social histories, as well as current medications. The tutorial aims to provide a clear understanding of this organized note-taking approach.