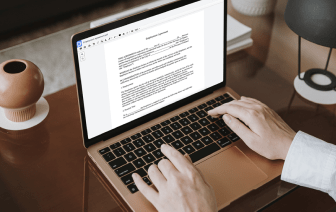
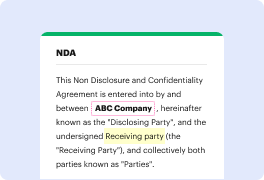
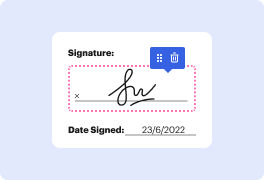
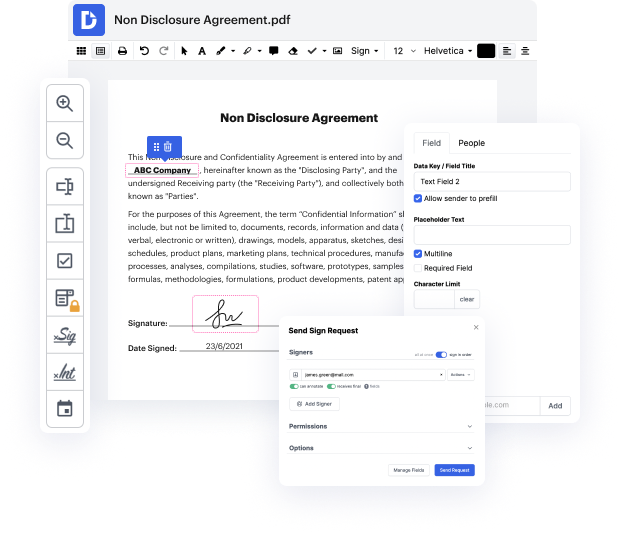
Handling and executing documents can be monotonous, but it doesn’t have to be. No matter if you need help daily or only sometimes, DocHub is here to equip your document-based projects with an extra performance boost. Edit, comment, fill in, sign, and collaborate on your Patient Progress Report rapidly and easily. You can alter text and images, build forms from scratch or pre-made templates, and add eSignatures. Owing to our high quality safety precautions, all your data stays secure and encrypted.
DocHub offers a comprehensive set of tools to streamline your paper processes. You can use our solution on multiple devices to access your work anywhere and whenever. Simplify your editing experience and save time of handiwork with DocHub. Try it for free right now!
hey guys doctor decide here from osmosis and I wanted to talk to you guys this week about how to write a really good progress note or clinical note and I brought with me a little prop so this is just to remind you uh what were talking about today and if youve written a note before you know why Im holding this up lets see if I can there it is s OAP subjective objective assessment and plan write soap or soap notes are what we call them sometimes and its just a shorthand from one remember kind of what what we should include in the note the subjective is what a patient tells you objective is kind of what you determined by yourself through physical exam or labs or imaging assessment is kind of thought process what do you think is going on and explaining that fully in a plan is just that its like what are you gonna do next so this is a soap note format its pretty universal and so this is what we want to talk about today what are my top three tips for writing a good note and this is ki