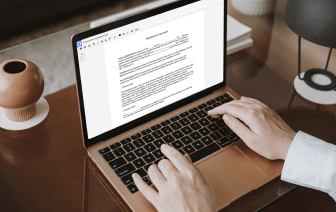
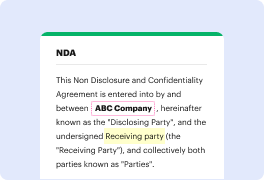
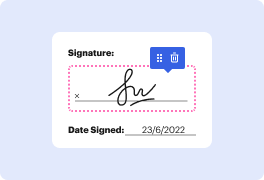
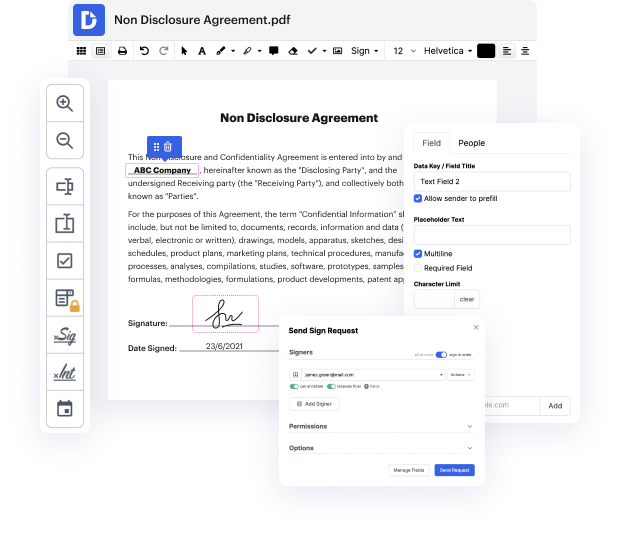
Time is a vital resource that every enterprise treasures and tries to transform in a reward. When picking document management software program, focus on a clutterless and user-friendly interface that empowers users. DocHub delivers cutting-edge features to optimize your file managing and transforms your PDF editing into a matter of one click. Replace Value Choice to the Soap Note with DocHub to save a lot of time as well as increase your productivity.
Make PDF editing an simple and intuitive process that saves you a lot of valuable time. Easily alter your files and give them for signing without having looking at third-party software. Focus on relevant tasks and increase your file managing with DocHub today.
In this tutorial, Dr. Decide from Osmosis discusses how to effectively write a clinical or progress note using the SOAP format. SOAP stands for Subjective, Objective, Assessment, and Plan. The subjective section includes information conveyed by the patient, while the objective section encompasses findings from physical exams, labs, or imaging. The assessment involves the clinician’s evaluation and thinking about the patient's condition, and the plan outlines the next steps in patient care. Dr. Decide aims to provide top three tips for writing an effective note, emphasizing the importance of clarity and thoroughness in each section.