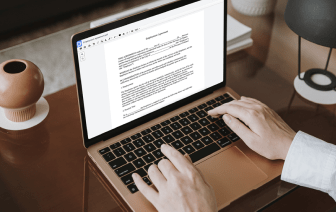

Time is an important resource that every company treasures and attempts to transform in a gain. When selecting document management software program, take note of a clutterless and user-friendly interface that empowers consumers. DocHub delivers cutting-edge tools to enhance your file administration and transforms your PDF file editing into a matter of a single click. Remove Calculations into the Soap Note with DocHub to save a lot of efforts and enhance your efficiency.
Make PDF file editing an simple and intuitive operation that helps save you plenty of valuable time. Quickly adjust your documents and send out them for signing without having switching to third-party solutions. Give attention to pertinent tasks and boost your file administration with DocHub today.
This video tutorial covers SOAP progress notes, a documentation method used by nurses and healthcare providers for patient charting. SOAP stands for Subjective, Objective, Assessment, and Plan. The "Subjective" component refers to the patient's own account of their experiences and feelings, including complaints and concerns. Examples include phrases like "The patient complains of feeling achy all over" or "The patient states a sore throat and chills started last night." This section should detail the onset, location, frequency, intensity, duration, and factors affecting the condition. For new patients, it is essential to include their medical, surgical, family, and social history, as well as current medications.