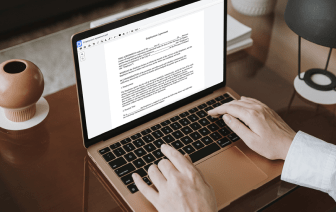
Document generation is a fundamental part of productive company communication and administration. You need an affordable and functional solution regardless of your document preparation point. Medical Claim preparation might be among those procedures which require additional care and consideration. Simply stated, you will find better options than manually producing documents for your small or medium company. One of the best approaches to make sure top quality and efficiency of your contracts and agreements is to adopt a multifunctional solution like DocHub.
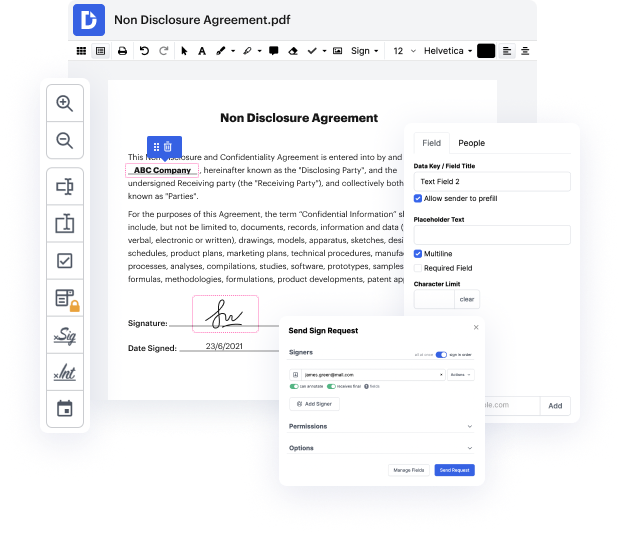
Editing flexibility is easily the most significant advantage of DocHub. Make use of robust multi-use instruments to add and take away, or modify any part of Medical Claim. Leave feedback, highlight important information, copy symbol in Medical Claim, and transform document managing into an easy and user-friendly procedure. Access your documents at any moment and apply new changes anytime you need to, which may substantially lower your time producing exactly the same document completely from scratch.
Create reusable Templates to make simpler your day-to-day routines and get away from copy-pasting exactly the same information continuously. Modify, add, and alter them at any moment to make sure you are on the same page with your partners and customers. DocHub helps you prevent errors in often-used documents and offers you the highest quality forms. Make sure that you always keep things professional and stay on brand with the most used documents.
Benefit from loss-free Medical Claim editing and protected document sharing and storage with DocHub. Do not lose any more files or end up perplexed or wrong-footed when discussing agreements and contracts. DocHub enables specialists anywhere to embrace digital transformation as part of their company’s change administration.
so this person has our job in billing and theyre a little bit nervous because those denials that means money coming in so thats a little bit nerve-racking making sure you get that money so when it comes in what are the steps to fixing that claim how do we get that claim gone so the denials come it could be a simple thing it could be complex so it all depends its going to depend on the denial so it could say youre you know one line item is tonight is inclusive and you look at it while its missing the modifier oops somebody missed a modifier they could just be requesting other health information or a primary EOB an accident detail form those could be classified as denials even though they didnt theyre not processing the claim yet because theyre requesting other information so denial is kind of a loose term that we use anything thats not paid is pretty much denied but theres suspended claims theres pending claims theyre not all denied or you could have that ever-important med