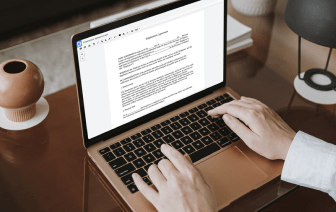
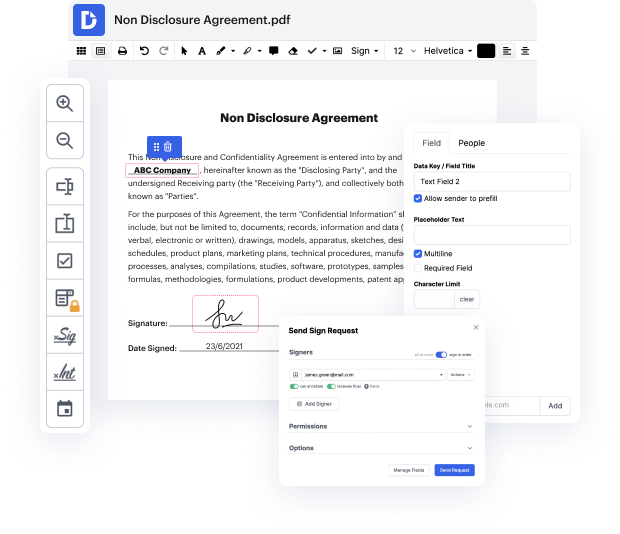
Need to quickly clean drawing in Patient Progress Report? Your search is over - DocHub offers the answer! You can get the work done fast without downloading and installing any software. Whether you use it on your mobile phone or desktop browser, DocHub enables you to modify Patient Progress Report anytime, at any place. Our versatile solution comes with basic and advanced editing, annotating, and security features, ideal for individuals and small businesses. We also offer plenty of tutorials and guides to make your first experience productive. Here's an example of one!
You don't need to worry about data safety when it comes to Patient Progress Report modifying. We provide such protection options to keep your sensitive data safe and secure as folder encryption, two-factor authentication, and Audit Trail, the latter of which tracks all your actions in your document.
In this tutorial, Dr. Decide from Osmosis discusses how to write an effective clinical note, specifically focusing on the SOAP note format. SOAP stands for Subjective, Objective, Assessment, and Plan. The Subjective section includes the patient's statements, while Objective encompasses findings from physical examinations, labs, or imaging. The Assessment details the clinician's thought process about the diagnosis, and the Plan outlines next steps in patient care. Dr. Decide intends to share his top three tips for creating a quality SOAP note, emphasizing the format's universality and importance in clinical documentation.